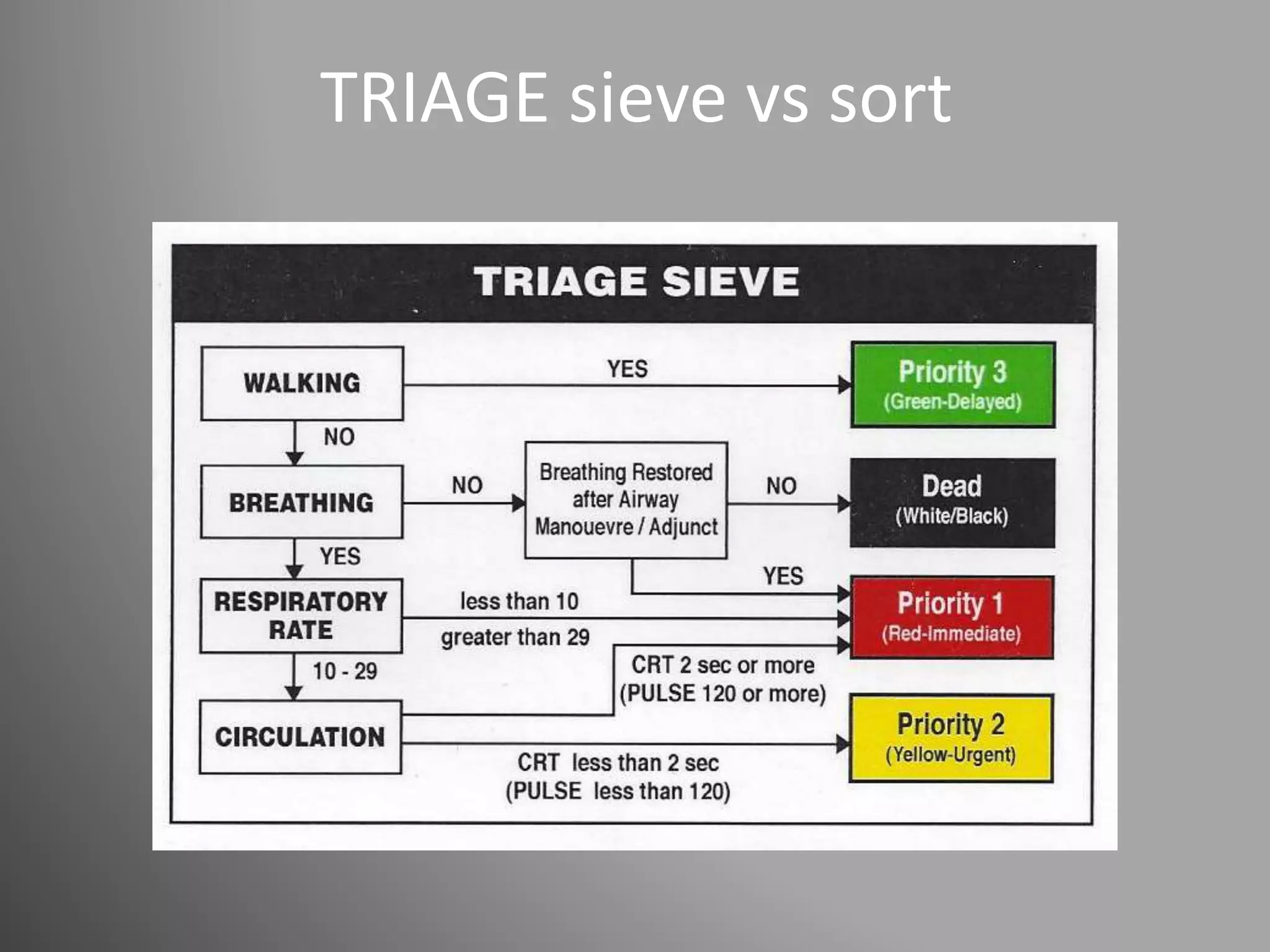
The document outlines the emergency department's response plan for a "Code Brown", which refers to mass casualty incidents that exceed the hospital's normal capacity. The 4 phases of response are notification, standby/preparation, reception of casualties, and stand down. Key steps include activating staff call backs, setting up triage and treatment areas, prioritizing patient care, and addressing issues like family inquiries, transportation bottlenecks, and media relations. The plan emphasizes timely triage, treatment and flow of patients. A post-incident debriefing within 7 days allows for evaluating the response and making improvements.