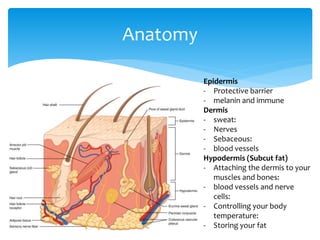
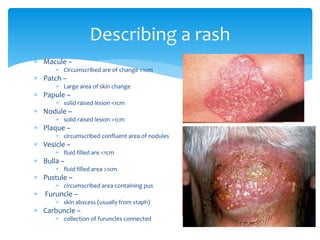
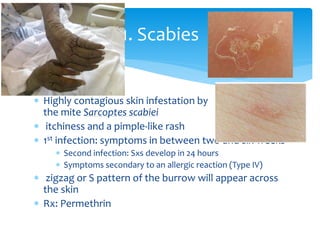
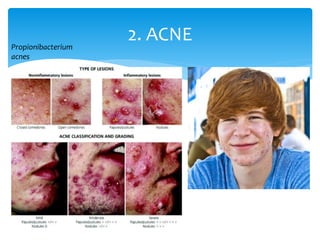
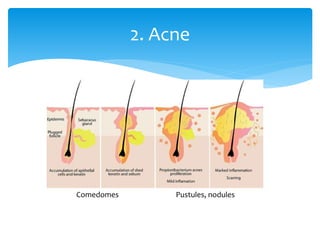
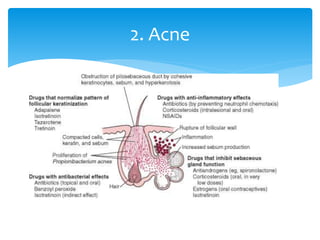
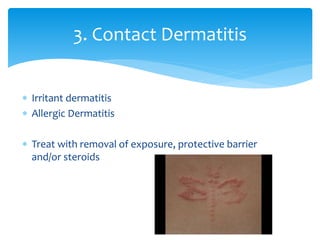
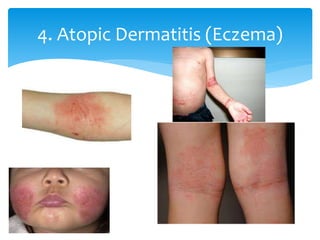
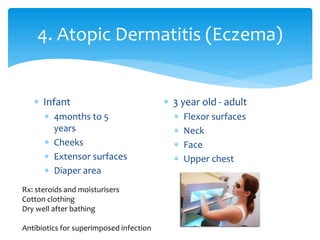
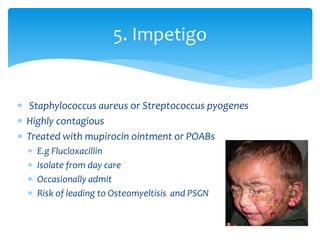
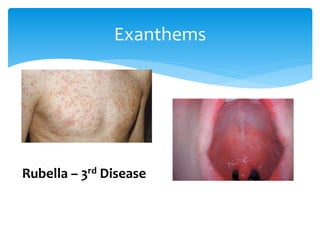
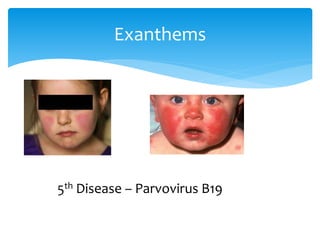
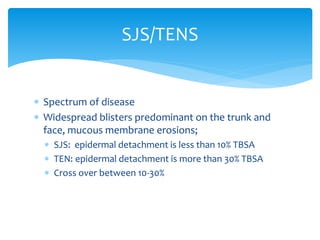
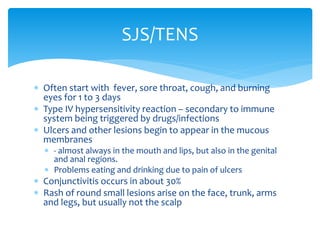
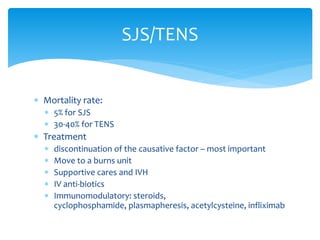
This document provides an overview of common paediatric rashes. It begins with describing the anatomy of the skin and definitions of common rash morphologies such as macules, papules, vesicles and pustules. Common rashes that are described include scabies, acne, contact dermatitis, atopic dermatitis, impetigo, tinea and nonspecific viral rashes. Specific viral exanthems like measles, rubella and scarlet fever are also reviewed. Emergent rashes like erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis are discussed in terms of their presentations, causes and treatments. References are provided at the end.