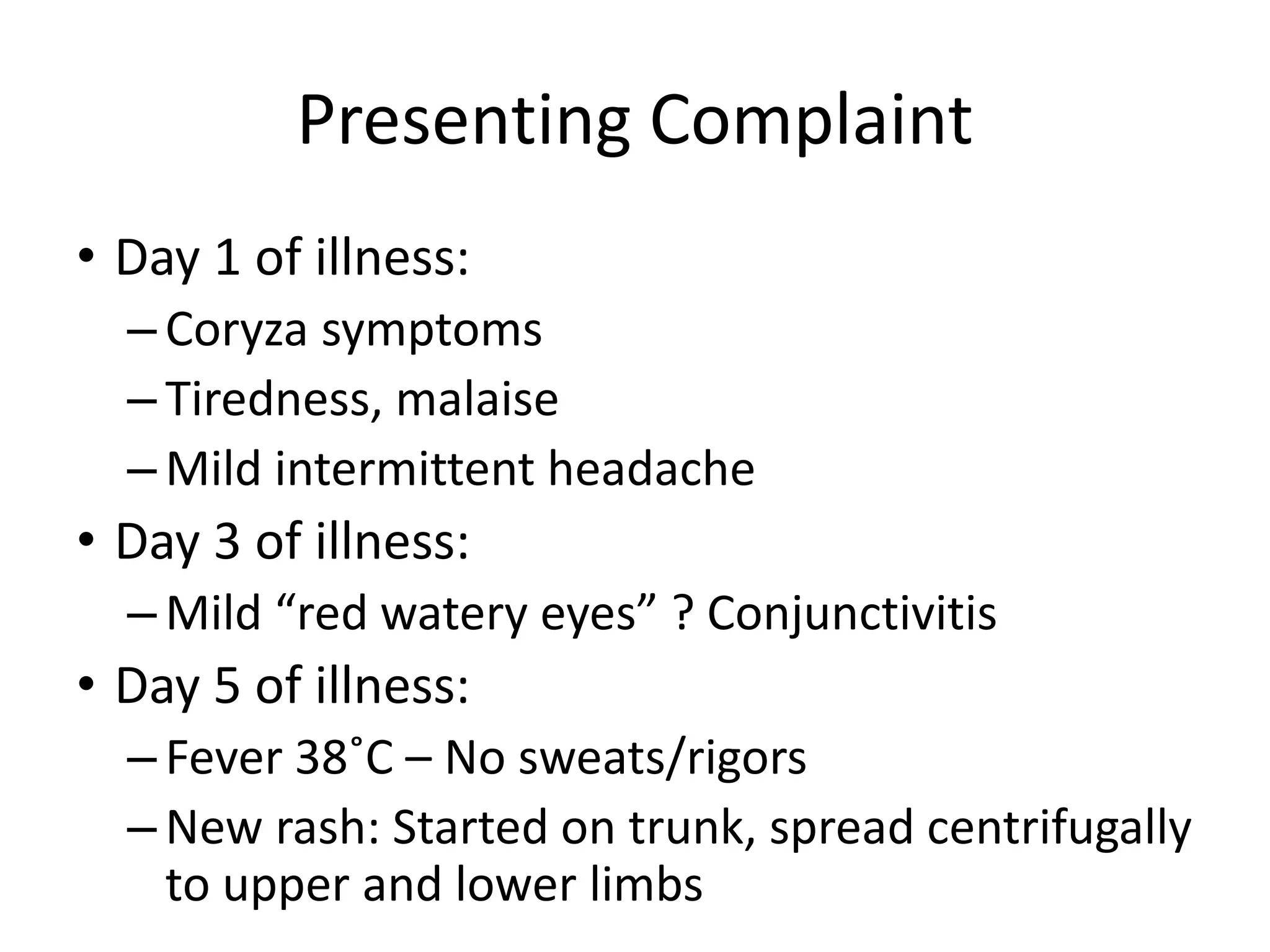
This document summarizes a case study of a 28-year-old Australian woman who developed a rash and respiratory symptoms after returning from travel to Thailand. Initial testing ruled out common infections like malaria, dengue fever, and influenza. Her rash and symptoms were consistent with measles. Further diagnostic testing confirmed infection with herpes simplex virus 1 via a positive PCR test. The case highlights the importance of considering uncommon infections in returning travelers who present with rashes and respiratory symptoms.