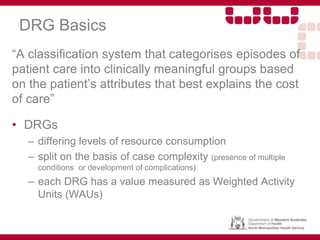
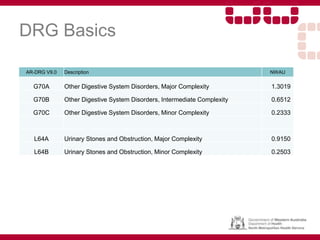
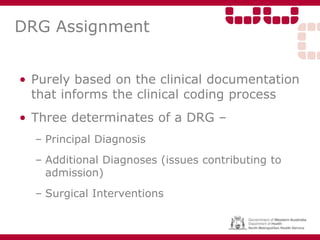
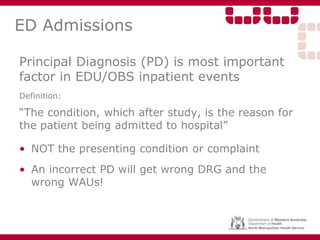
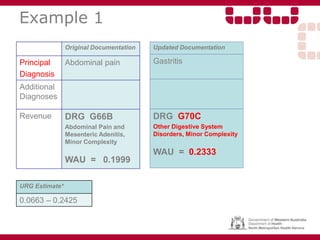
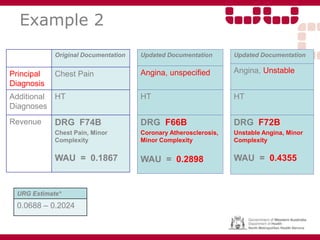
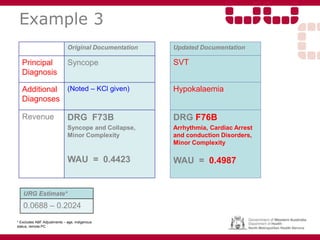
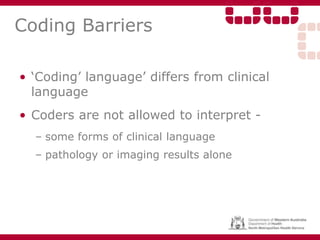
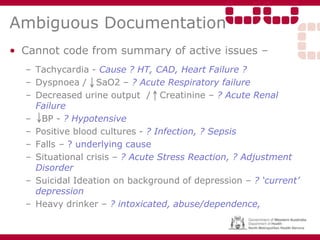
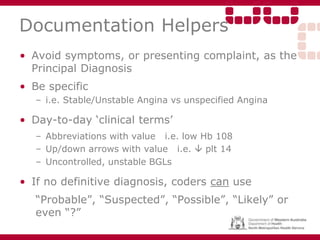
Good clinical documentation is critical for continuity of patient care, patient safety, legal records, and supporting accurate medical coding. The documentation provides information on why the patient was admitted and what treatments they received. The coders assign diagnosis and procedure codes based solely on the documented information. Ambiguous or incomplete documentation can result in inaccurate coding that affects funding. Ensuring documentation clearly specifies diagnoses, management plans, and interventions helps ensure patients are assigned to the appropriate Diagnosis Related Group (DRG) and the hospital receives appropriate funding for the services provided.