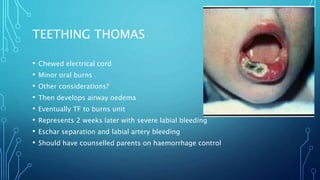
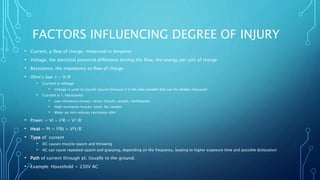
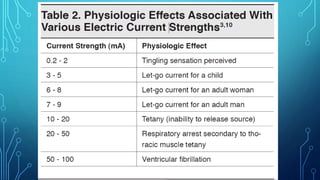
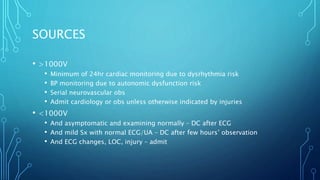
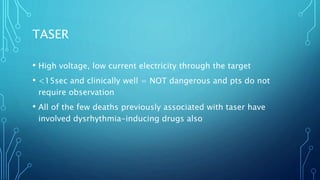
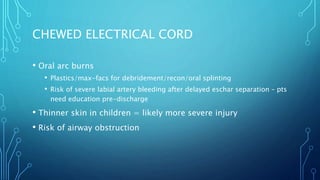
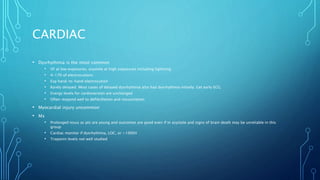
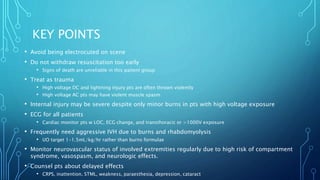
- This document contains information on various electrical injury cases presented to the emergency department, including details on mechanisms of injury, clinical presentations, investigations, and management strategies. Key points include treating electrical injury patients as trauma patients, avoiding premature withdrawal of resuscitation due to the unreliable signs of death, monitoring for cardiac dysrhythmias, rhabdomyolysis, and neurovascular compromise of injured extremities. High voltage or lightning injuries can cause severe internal injuries despite minor external burns and require prolonged cardiac monitoring and aggressive IV fluid resuscitation.