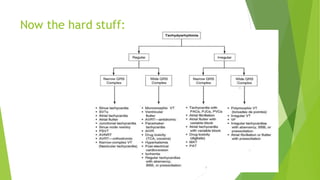
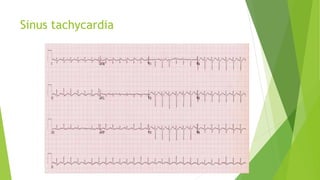
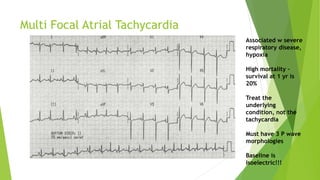
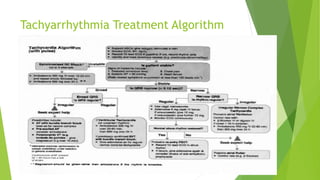
This document discusses various tachyarrhythmias, including:
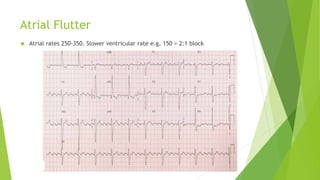
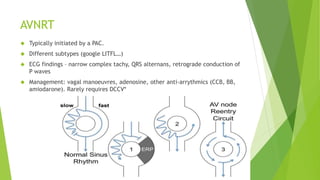
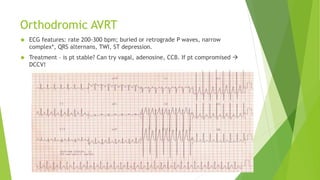
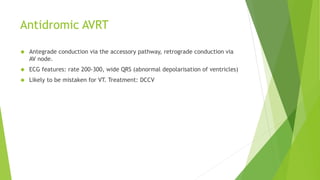
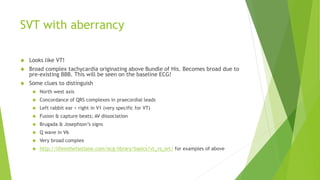
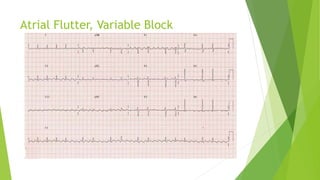
- Supraventricular tachycardias like atrial flutter, AV nodal reentrant tachycardia, and AV reentrant tachycardia.
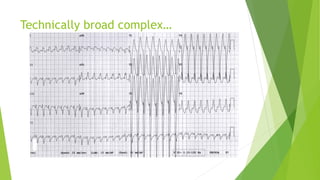
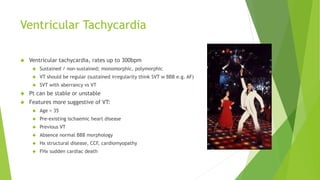
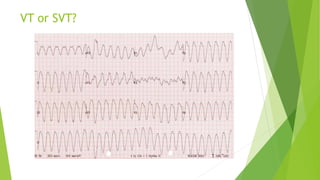
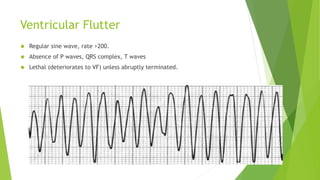
- Ventricular arrhythmias including ventricular tachycardia and ventricular flutter.
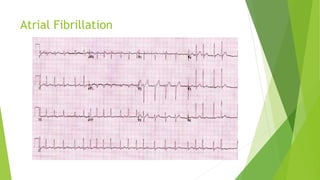
- Irregular rhythms such as atrial fibrillation.
It provides details on characteristics like rate, morphology, underlying causes, and treatment approaches for each type of tachycardia. Emphasis is placed on distinguishing ventricular tachycardia from supraventricular tachycardia with aberrancy in clinical evaluation.