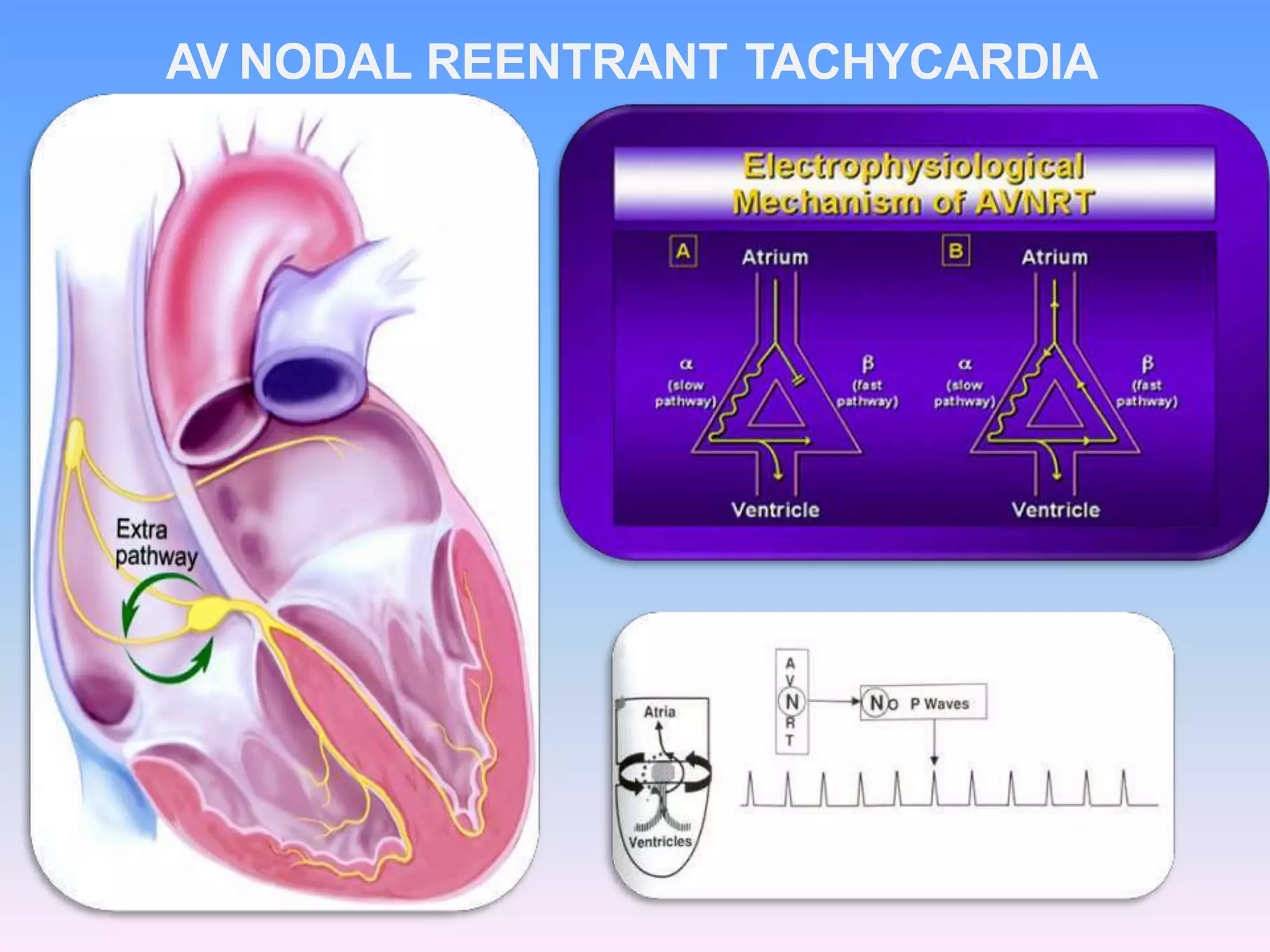
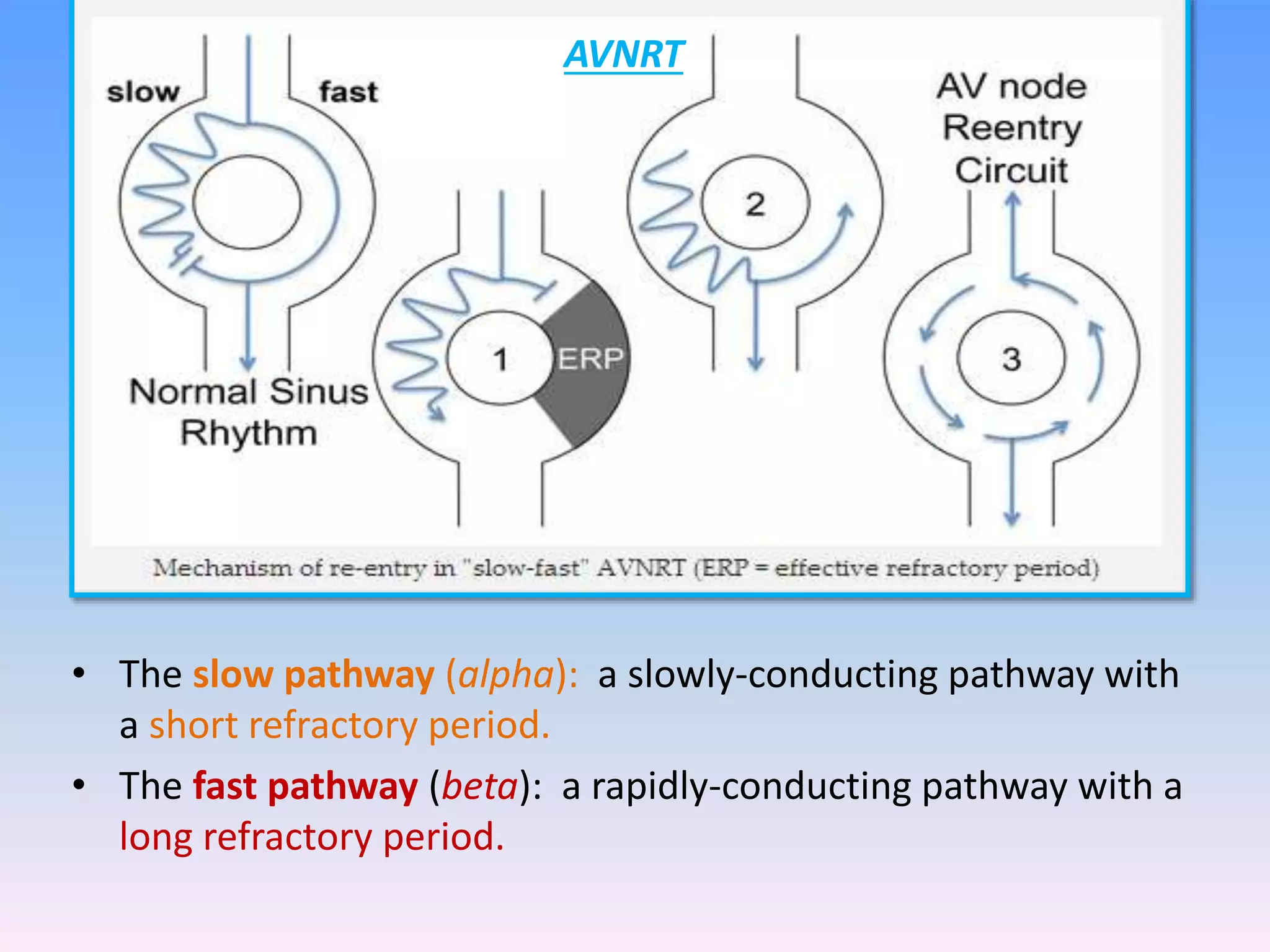
This document discusses the approach to evaluating and treating narrow complex tachycardia. It begins by describing the different mechanisms of tachyarrhythmias including enhanced automaticity, triggered automaticity, and reentry. It then discusses specific types of narrow complex tachycardia such as AV nodal reentrant tachycardia, AV reentrant tachycardia, atrial tachycardia, junctional ectopic tachycardia, and atrial flutter. It provides guidance on evaluating the ECG and patient response to determine the mechanism and appropriate treatment. Treatment options discussed include vagal maneuvers, adenosine, calcium channel blockers, beta blockers, and cardioversion for unstable patients.