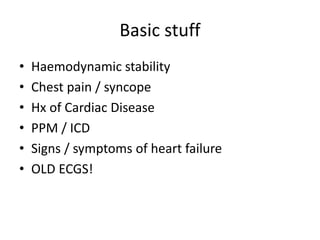
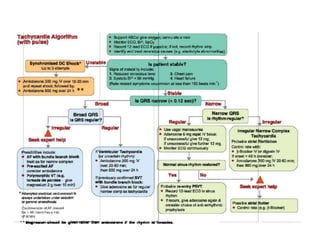
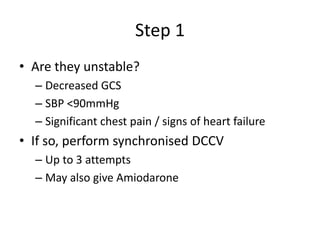
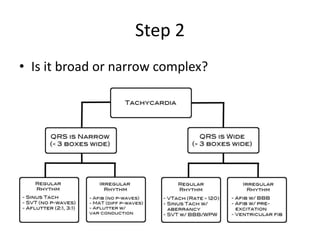
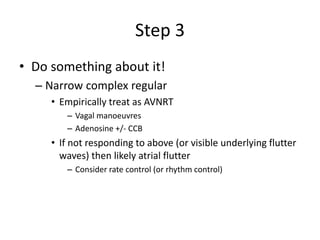
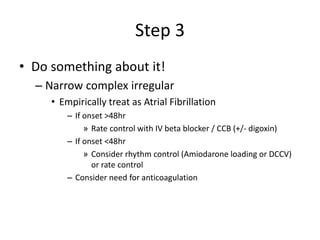
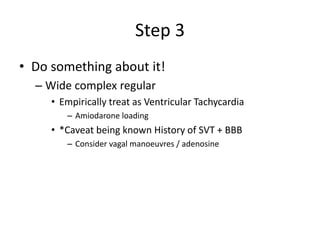
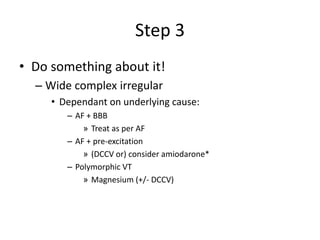
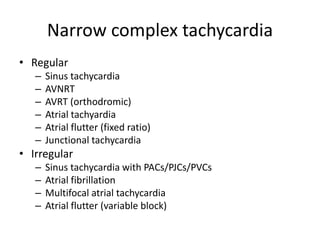
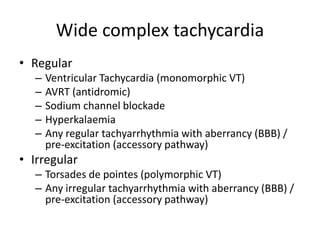
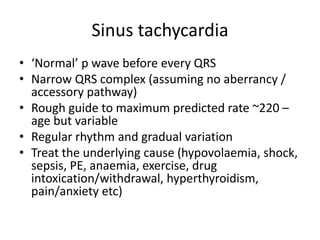
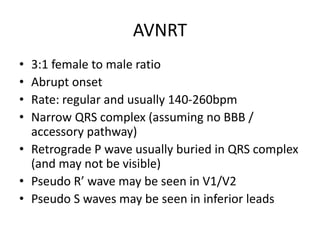
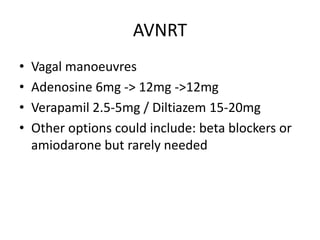
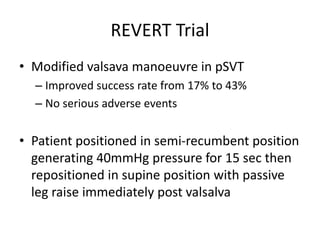
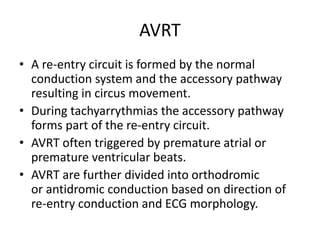
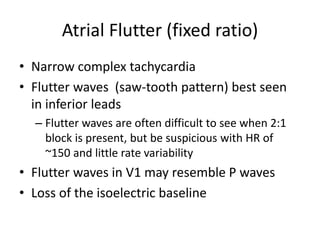
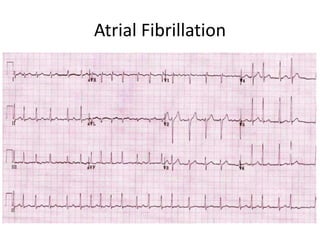
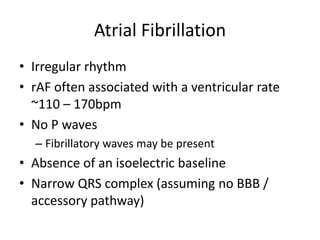
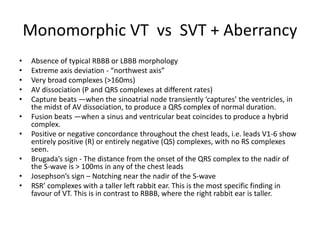
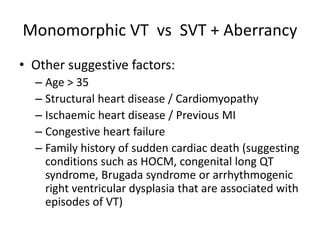
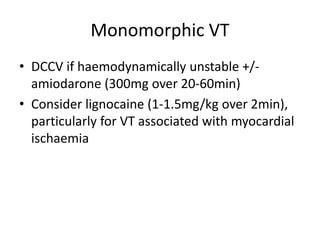
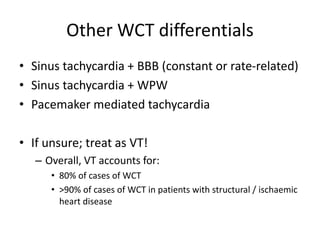
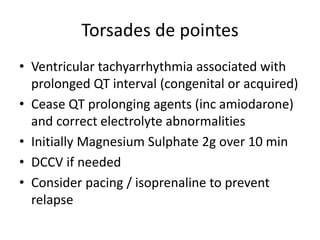
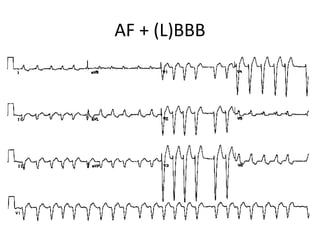
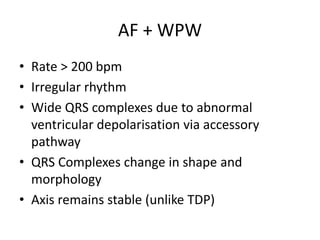
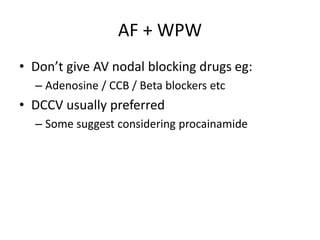
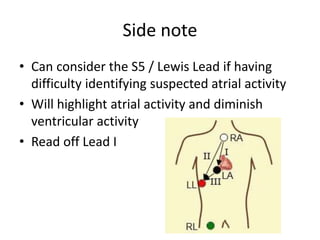
This document provides guidance on the assessment and treatment of arrhythmias presenting in the emergency department. It outlines an approach of first determining hemodynamic stability, then distinguishing between narrow and wide complex tachycardias, and finally determining the specific arrhythmia and appropriate treatment. For unstable patients with any arrhythmia, synchronized direct current cardioversion is recommended. Further treatment is tailored based on whether the arrhythmia has narrow or wide QRS complexes and is regular or irregular.