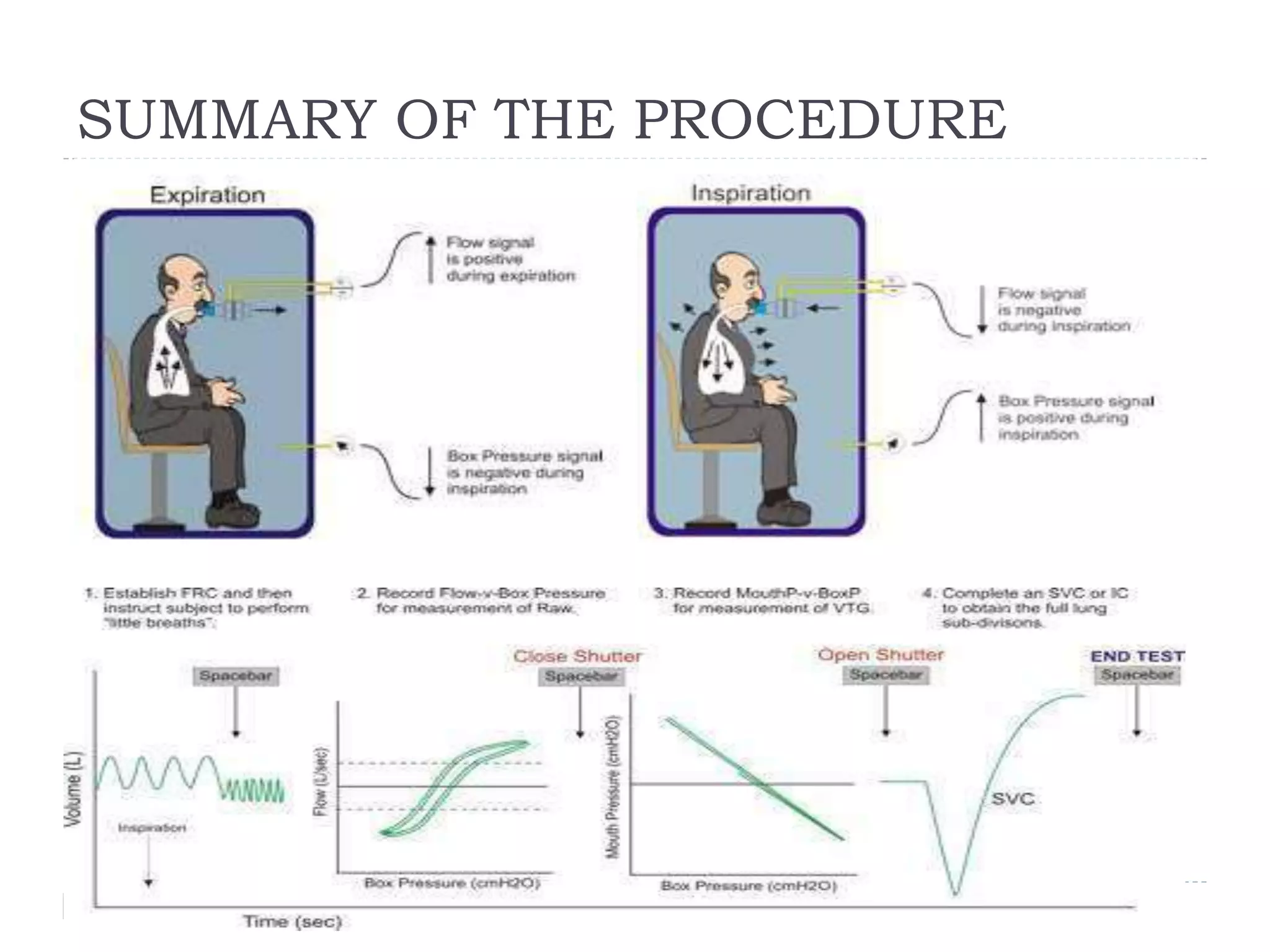
Body plethysmography is a technique used to measure lung volumes like intrathoracic gas volume (TGV) and airway resistance. It involves having the patient breathe in an enclosed chamber while measuring changes in pressure and volume. Specific airway resistance (sRaw) is determined from the relationship between respiratory flow and volume shifts in the chamber. Intrathoracic gas volume (ITGV) can also be measured by having the patient breathe against a shutter to create a closed system where changes in pressure and volume can estimate ITGV based on Boyle's law. Clinical applications include evaluating effects of pulmonary disorders on lung volumes like functional residual capacity (FRC) and residual volume (RV).