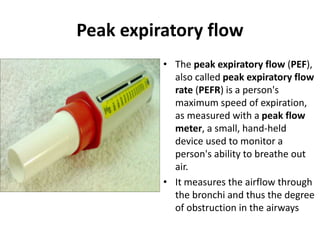
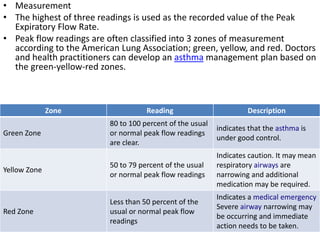
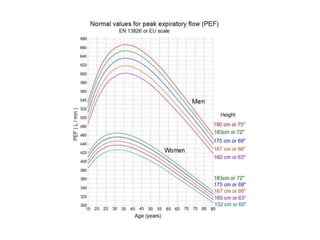
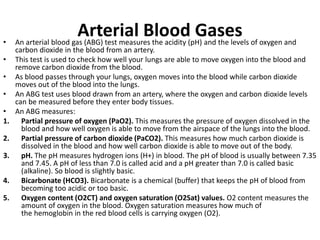
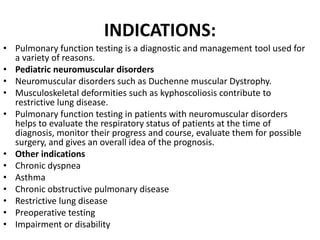
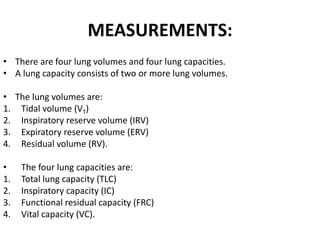
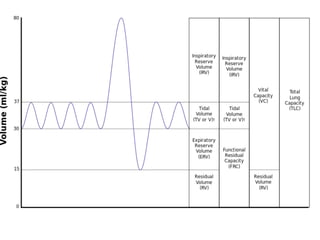
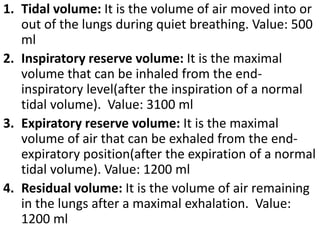
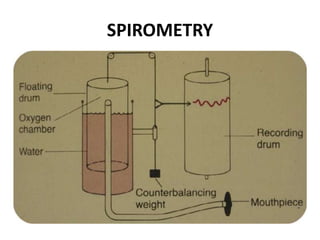
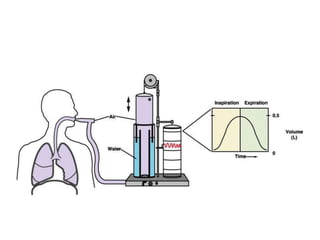
Pulmonary function tests evaluate lung function through measurements of lung volumes, capacities, flows, and gas exchange. Spirometry is the most common pulmonary function test and measures volumes of air inhaled and exhaled over time through the use of a spirometer. Key spirometry metrics include forced vital capacity, forced expiratory volume in 1 second, and peak expiratory flow rate. Arterial blood gases analyze blood pH, oxygen, and carbon dioxide levels to assess lung function and respiratory disease. Together, pulmonary function tests provide diagnostic and monitoring tools for conditions like asthma, COPD, and lung impairments.
![• Parameters
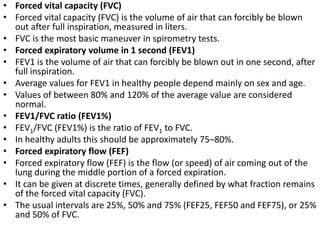
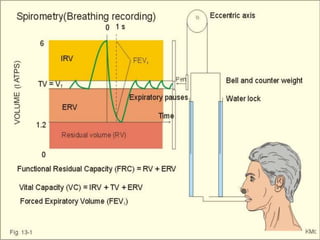
• The most common parameters measured in spirometry
are
1. Vital capacity (VC),
2. Forced vital capacity (FVC),
3. Forced expiratory volume (FEV) at timed intervals of
0.5, 1.0 (FEV1), 2.0, and 3.0 seconds,
4. Forced expiratory flow 25–75% (FEF 25–75) and
5. Maximal voluntary ventilation (MVV),[5] also known as
Maximum breathing capacity.
* Functional residual capacity (FRC) cannot be measured
via spirometry, but it can be measured with
a plethysmograph or dilution tests (for example, helium
dilution test)](https://image.slidesharecdn.com/pft-140904123628-phpapp01/85/Pulmonary-Function-Testing-Simplified-description-13-320.jpg)