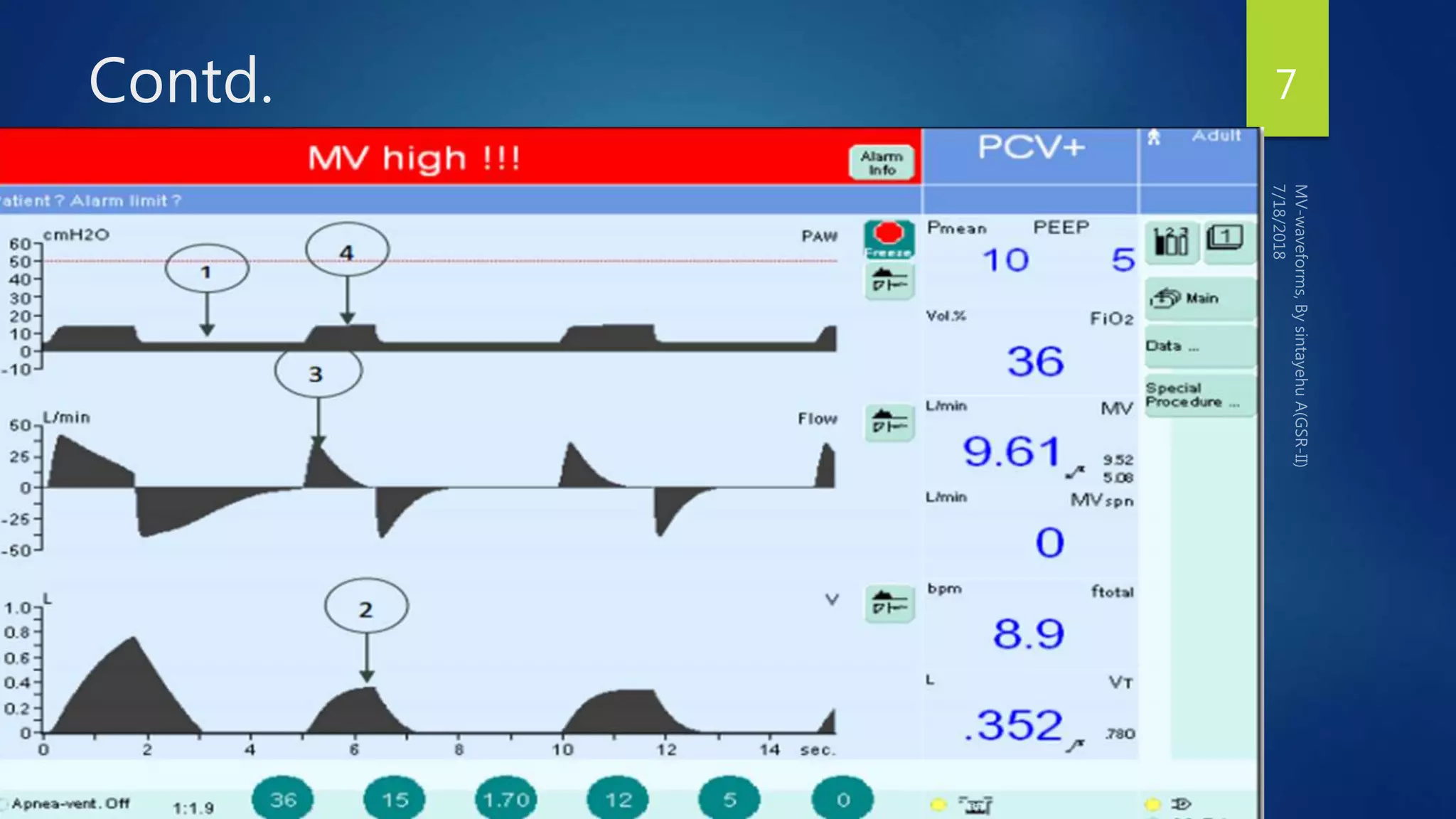
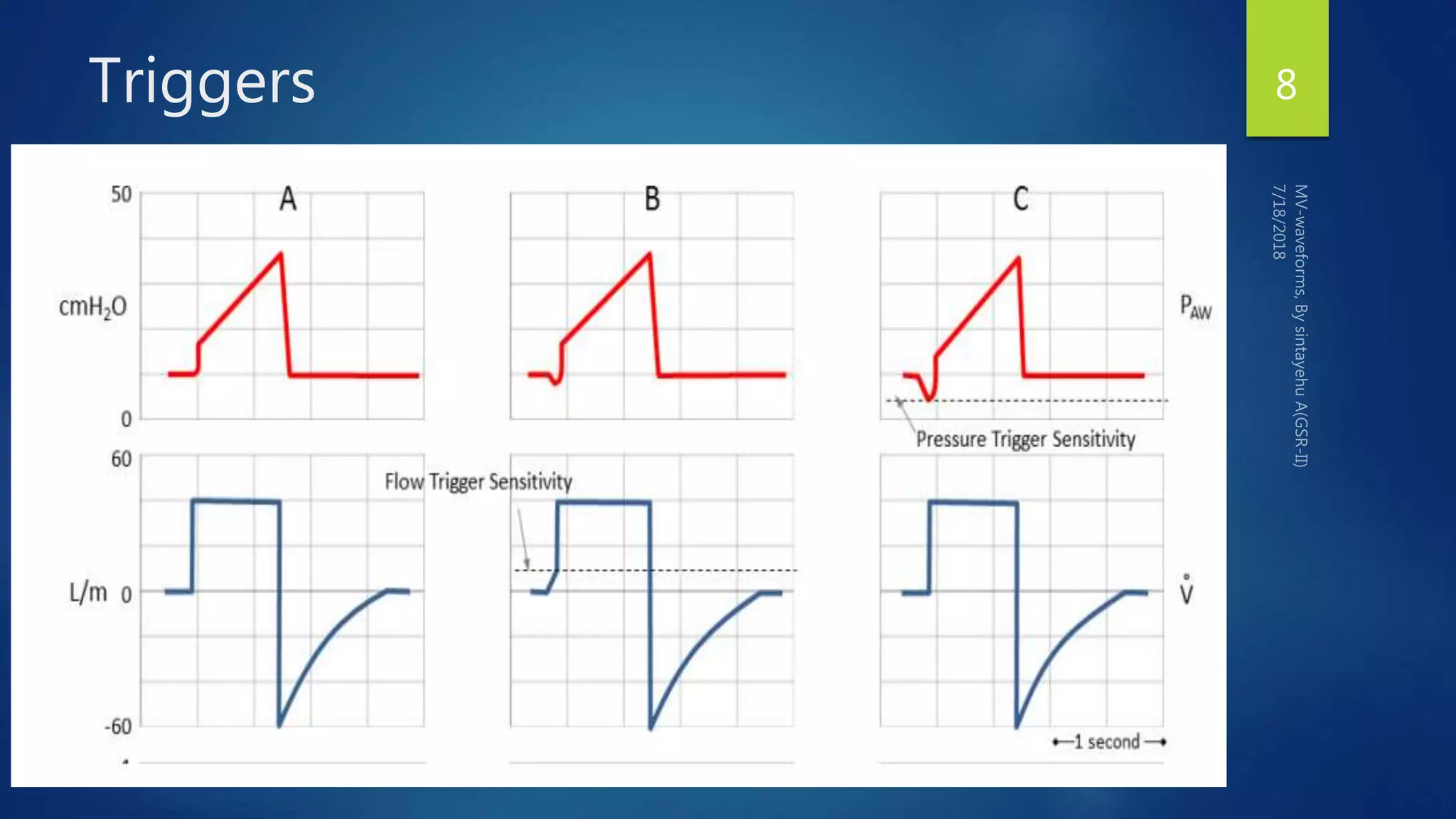
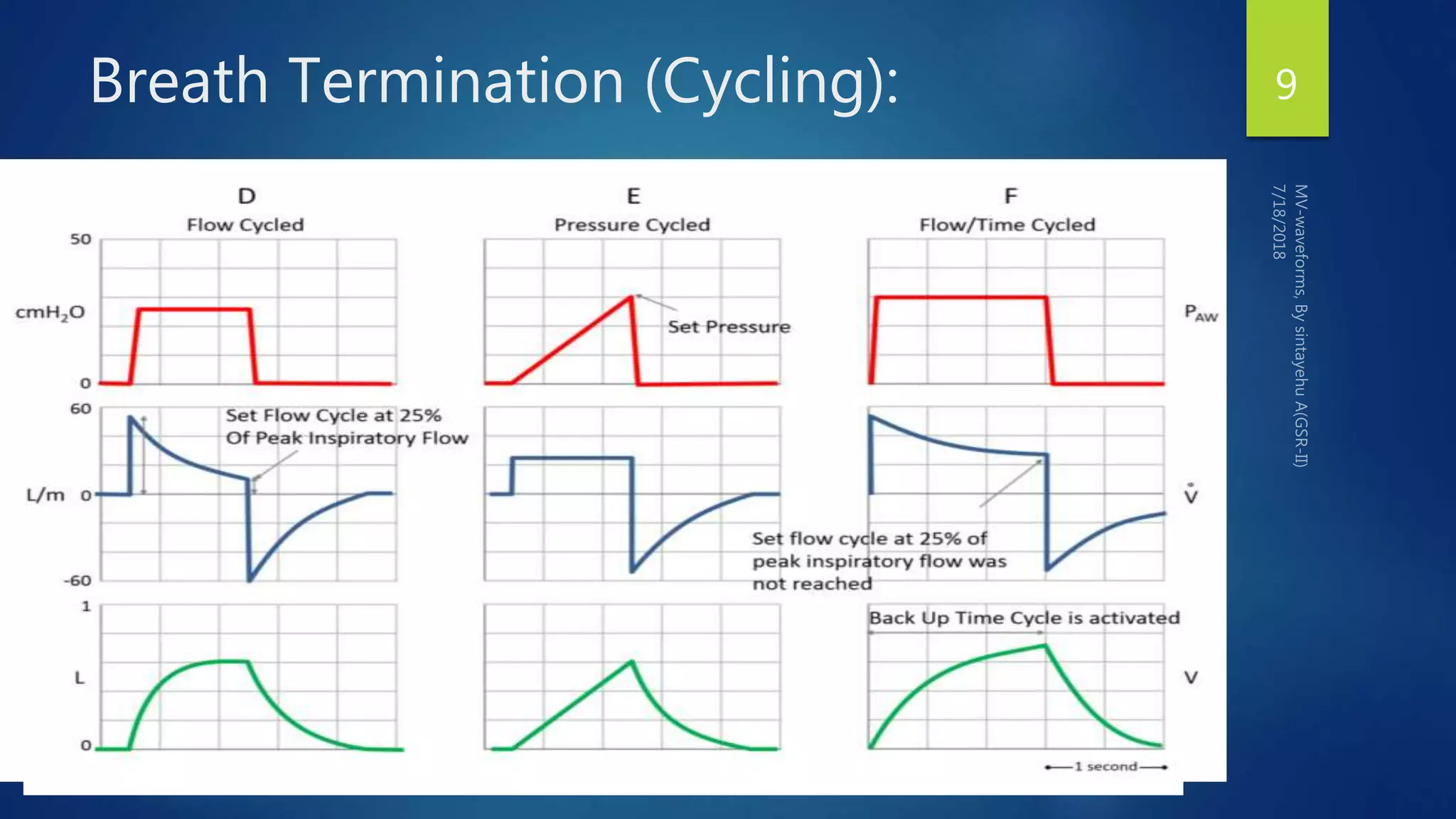
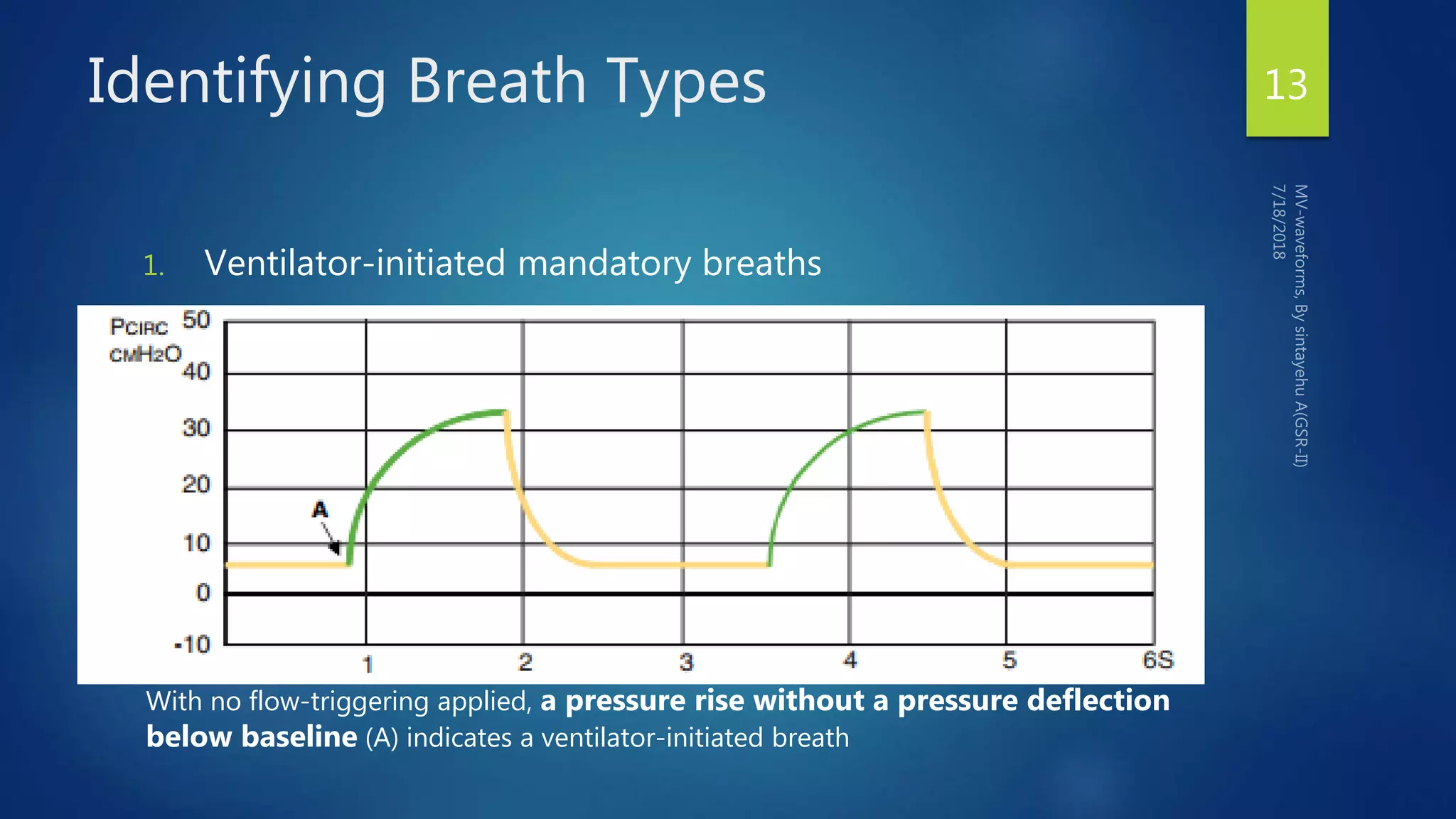
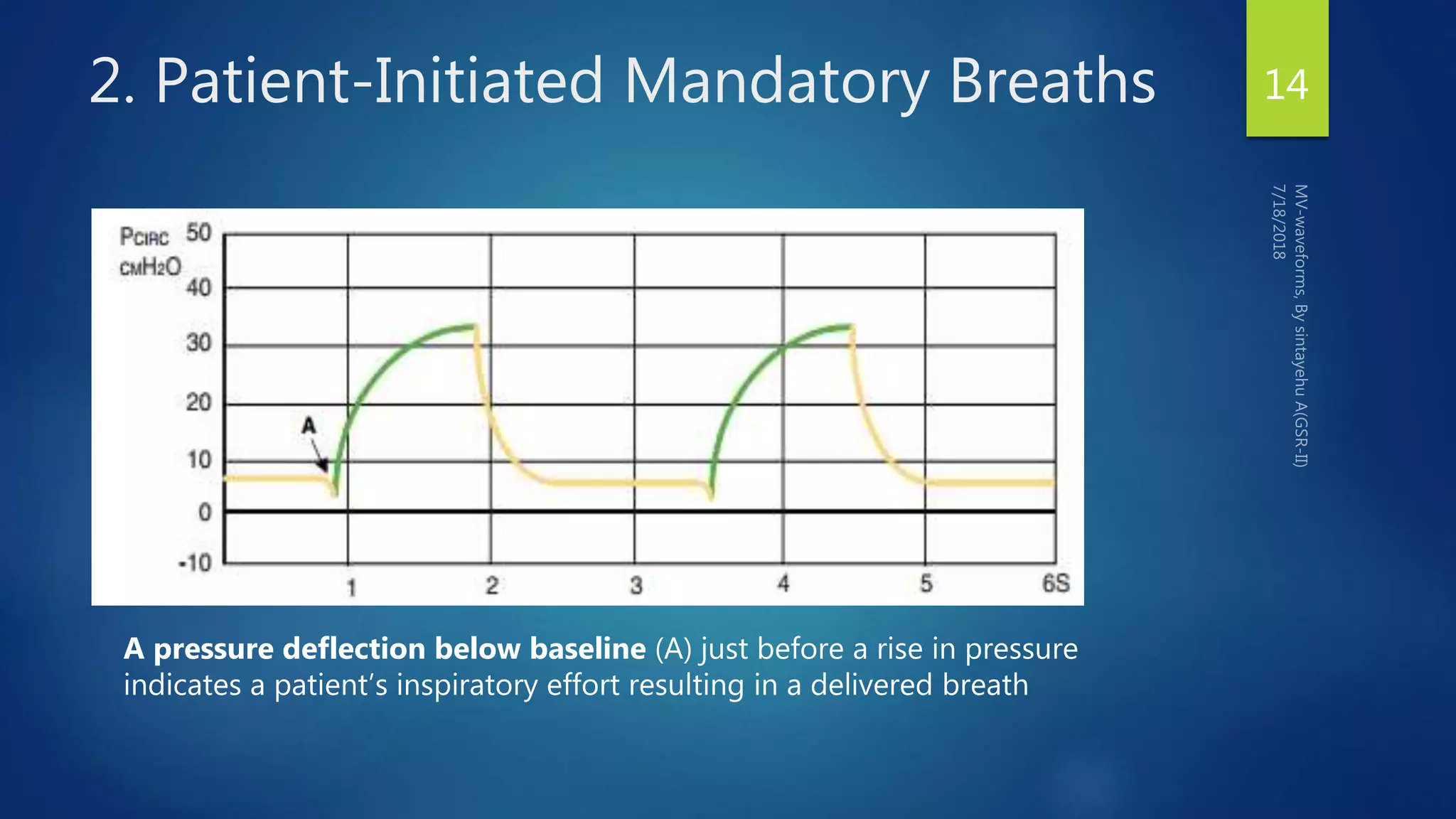
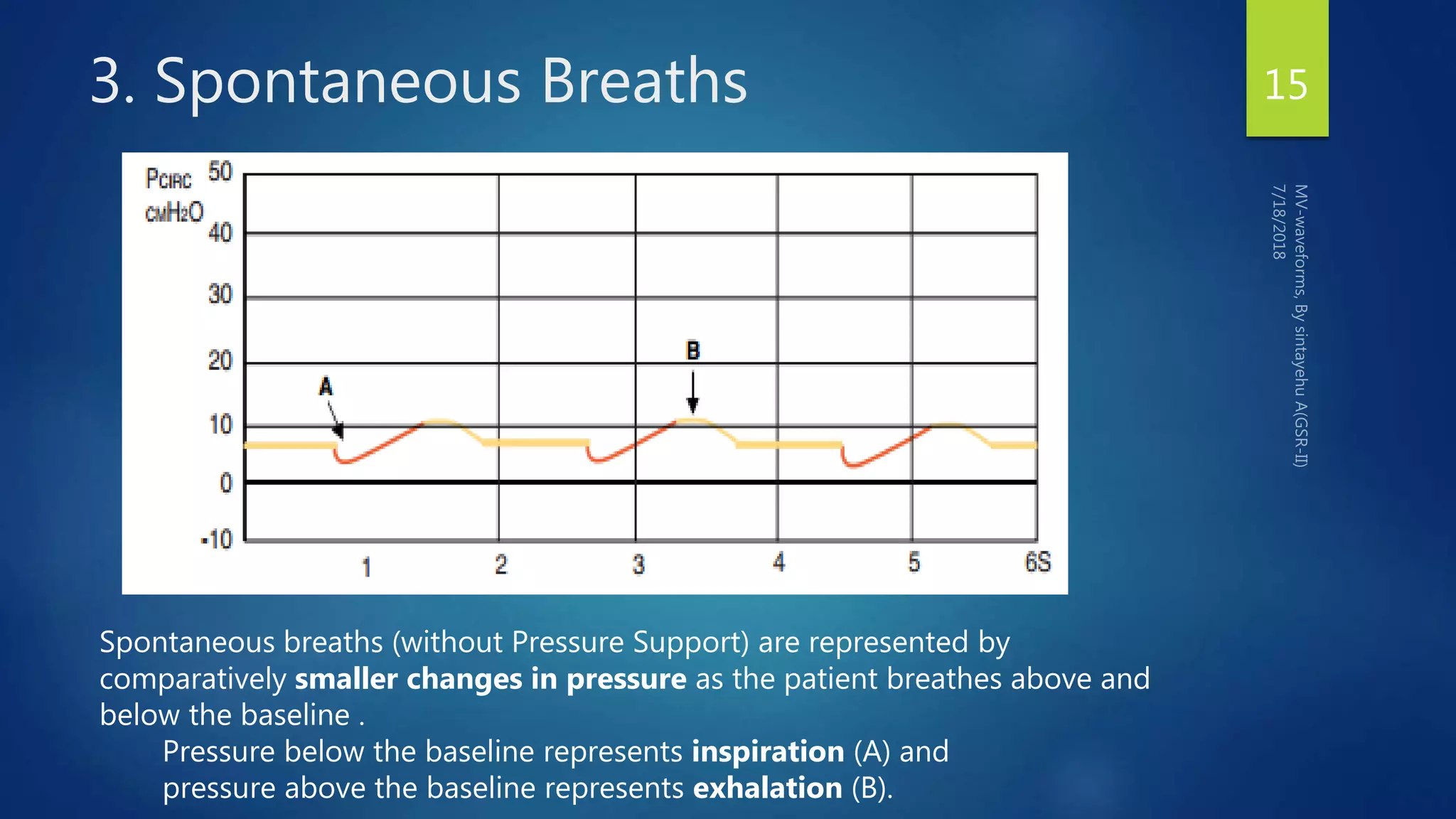
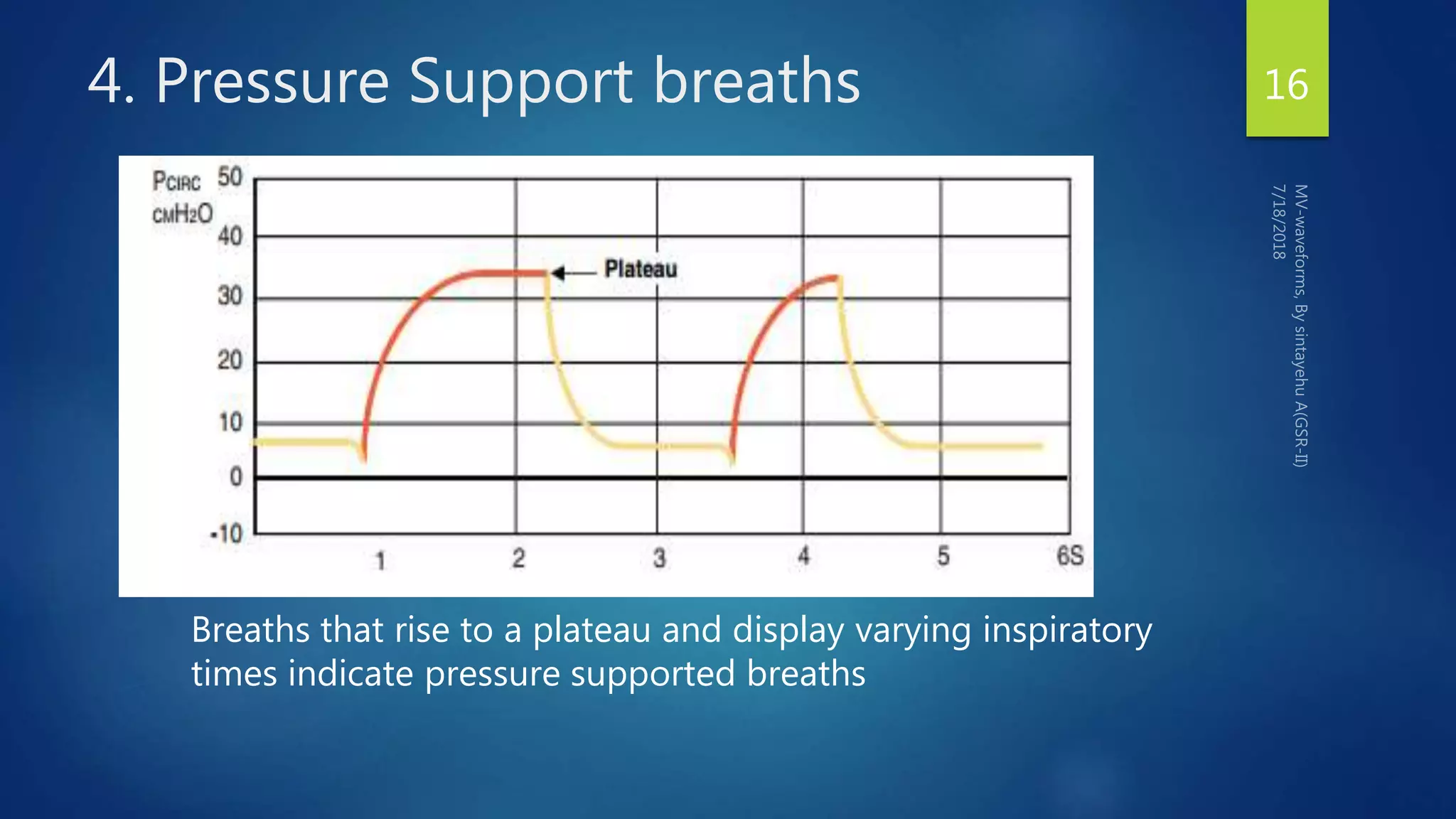
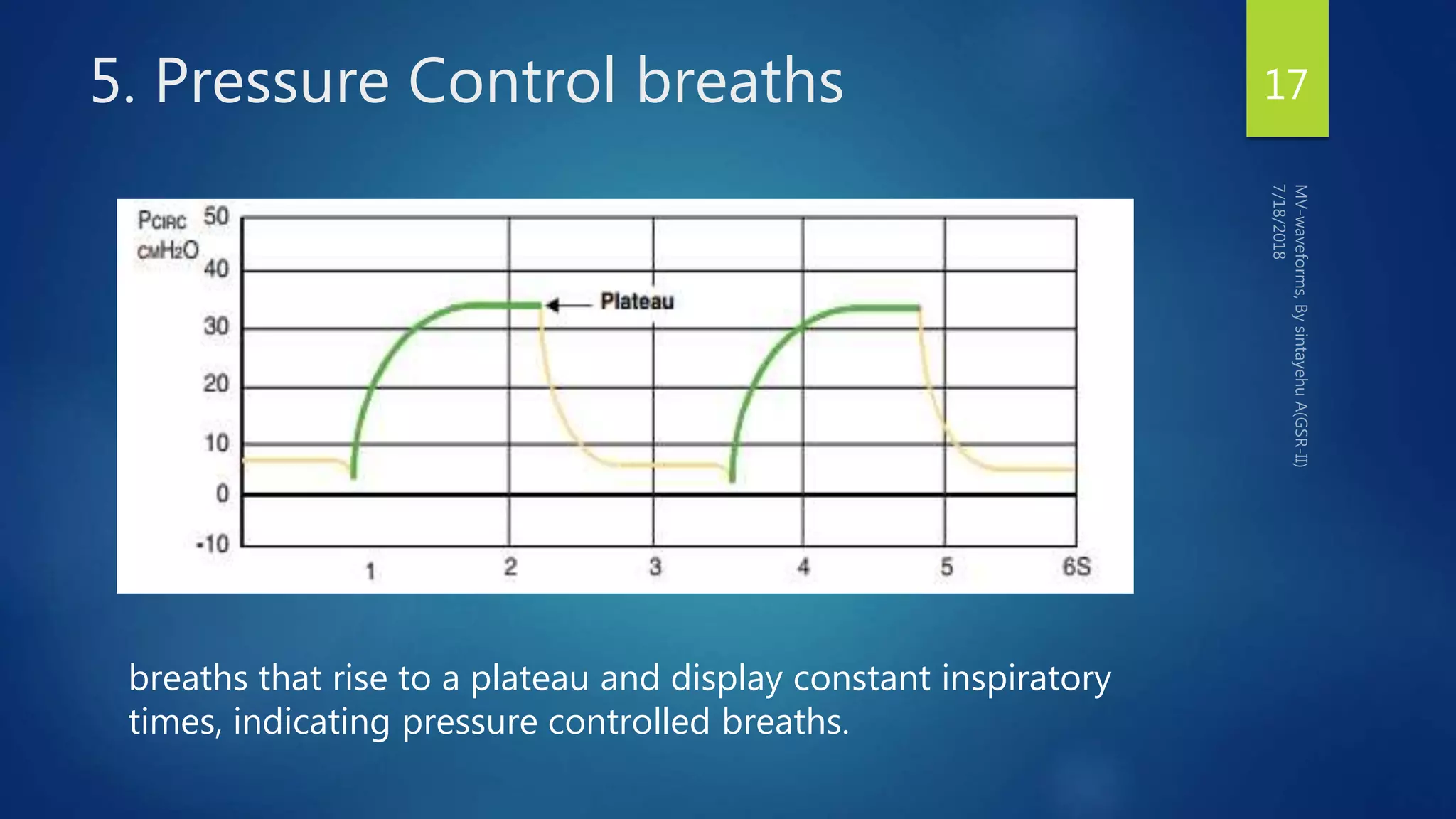
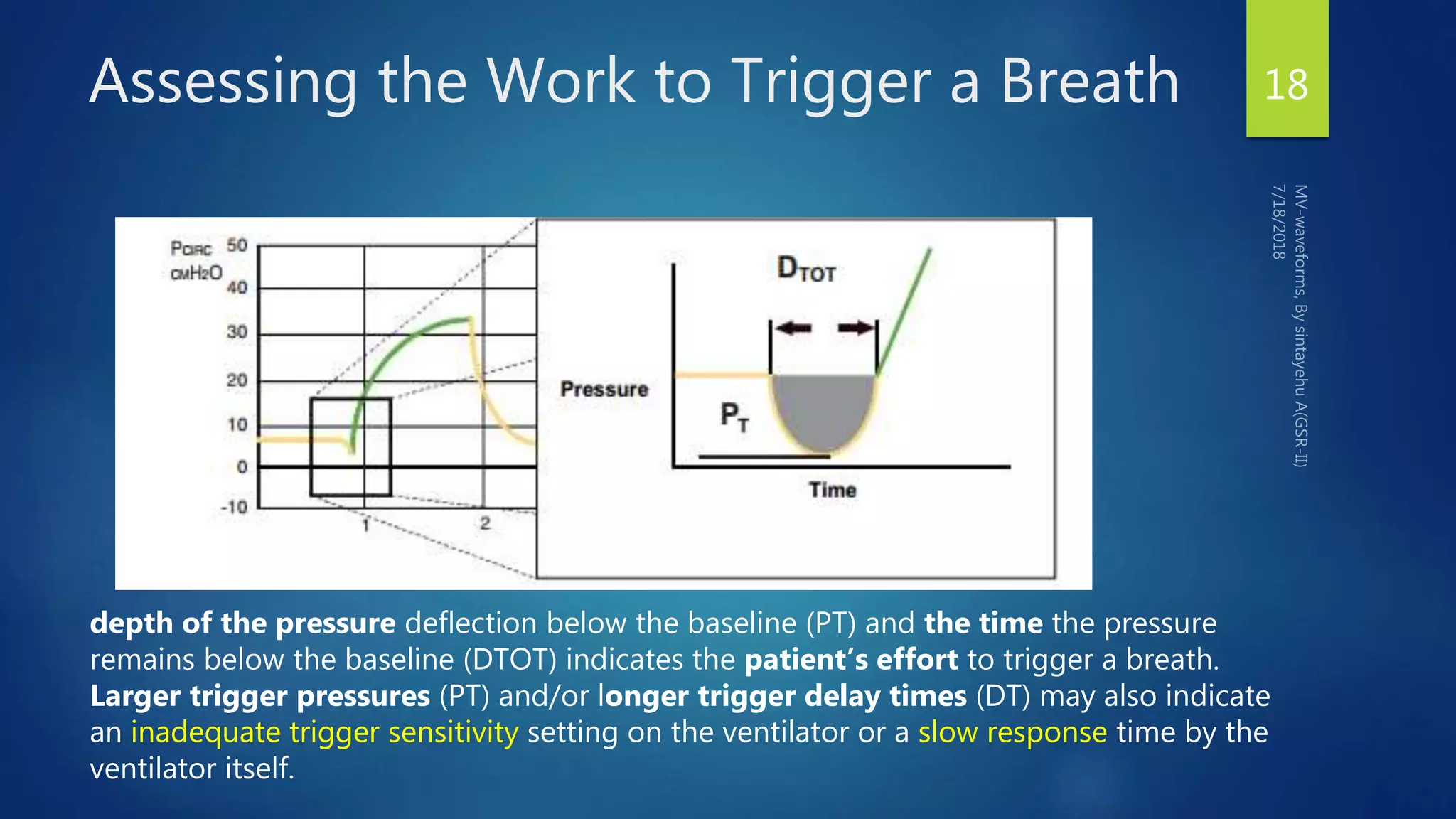
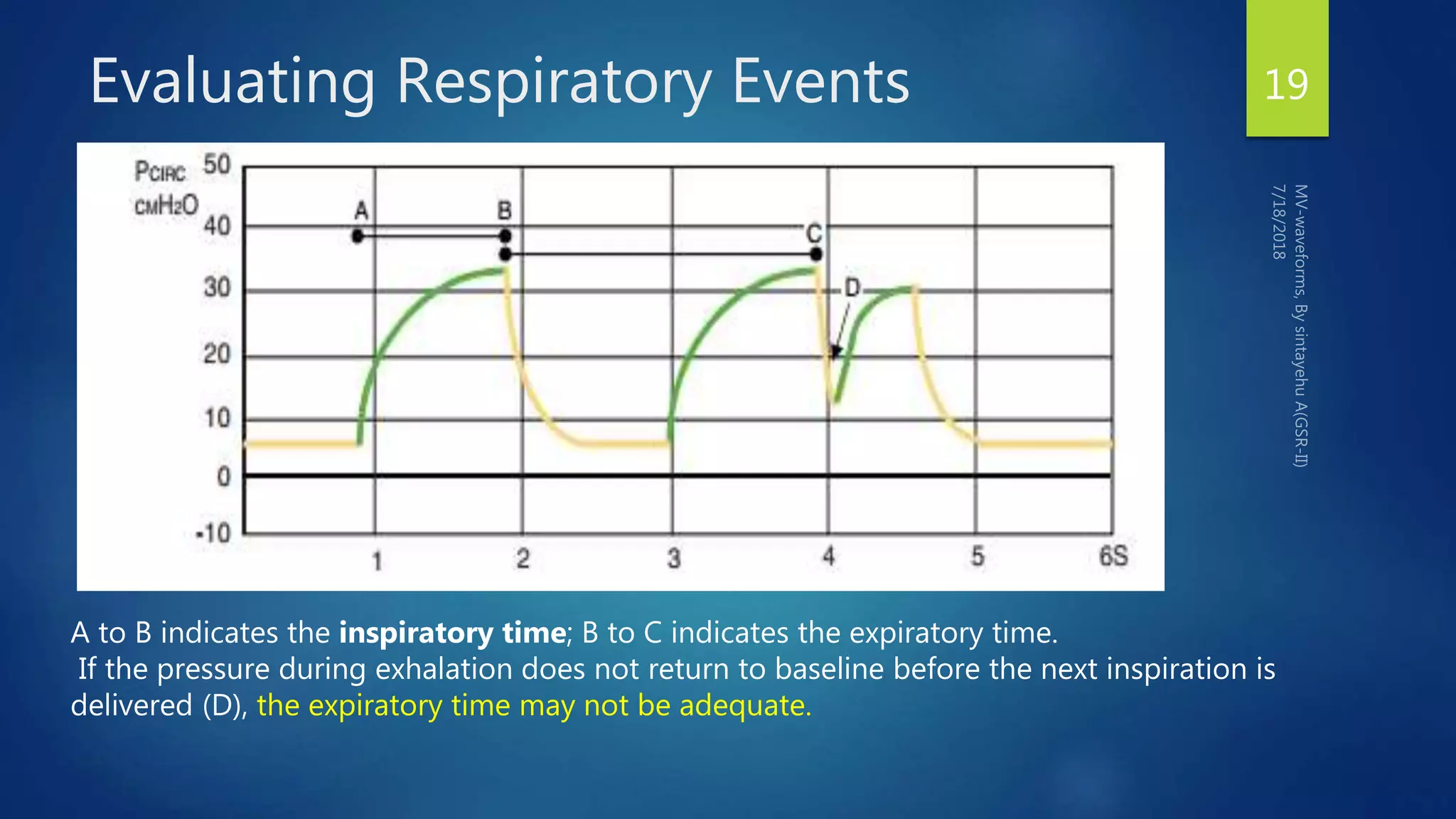
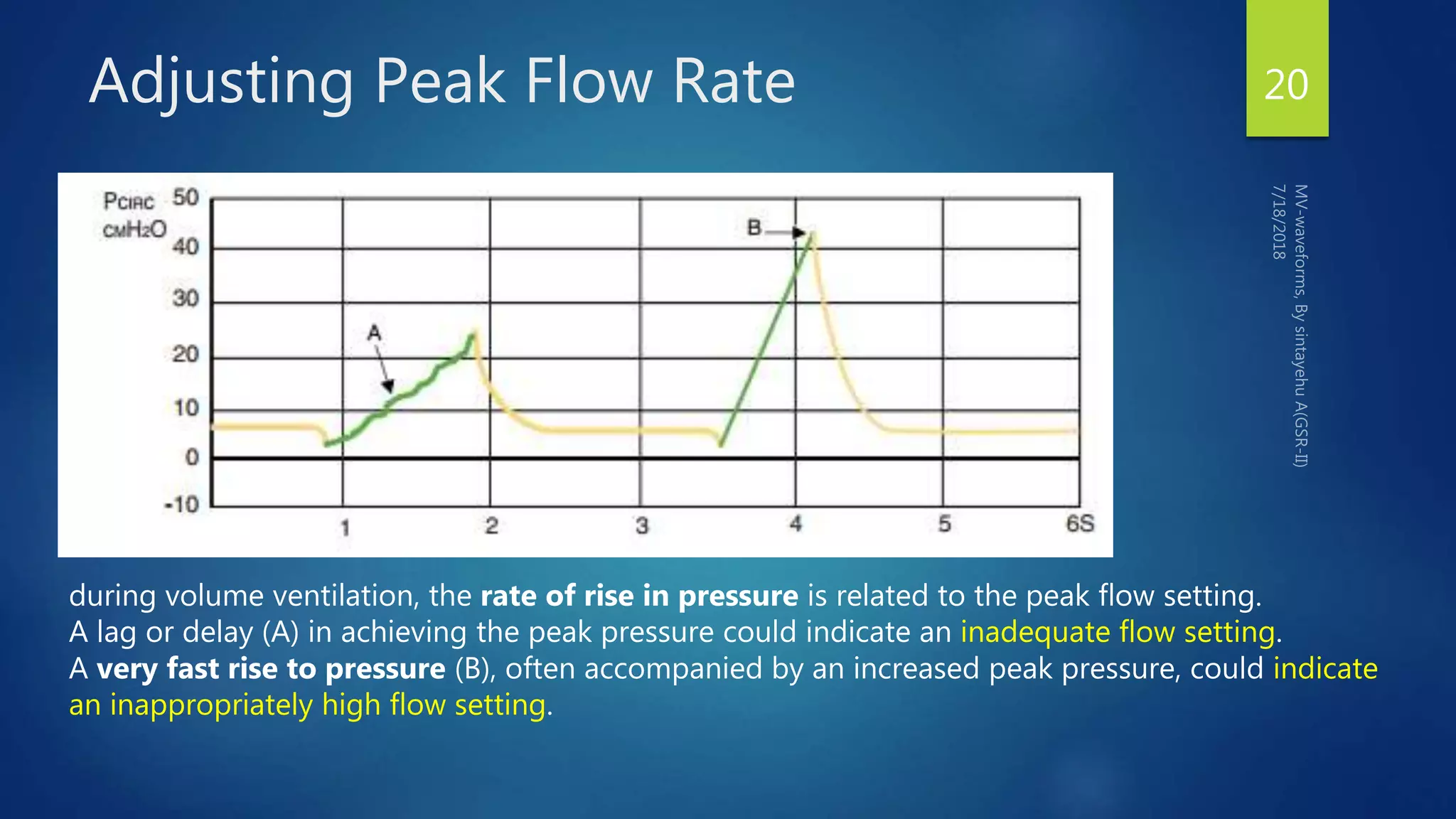
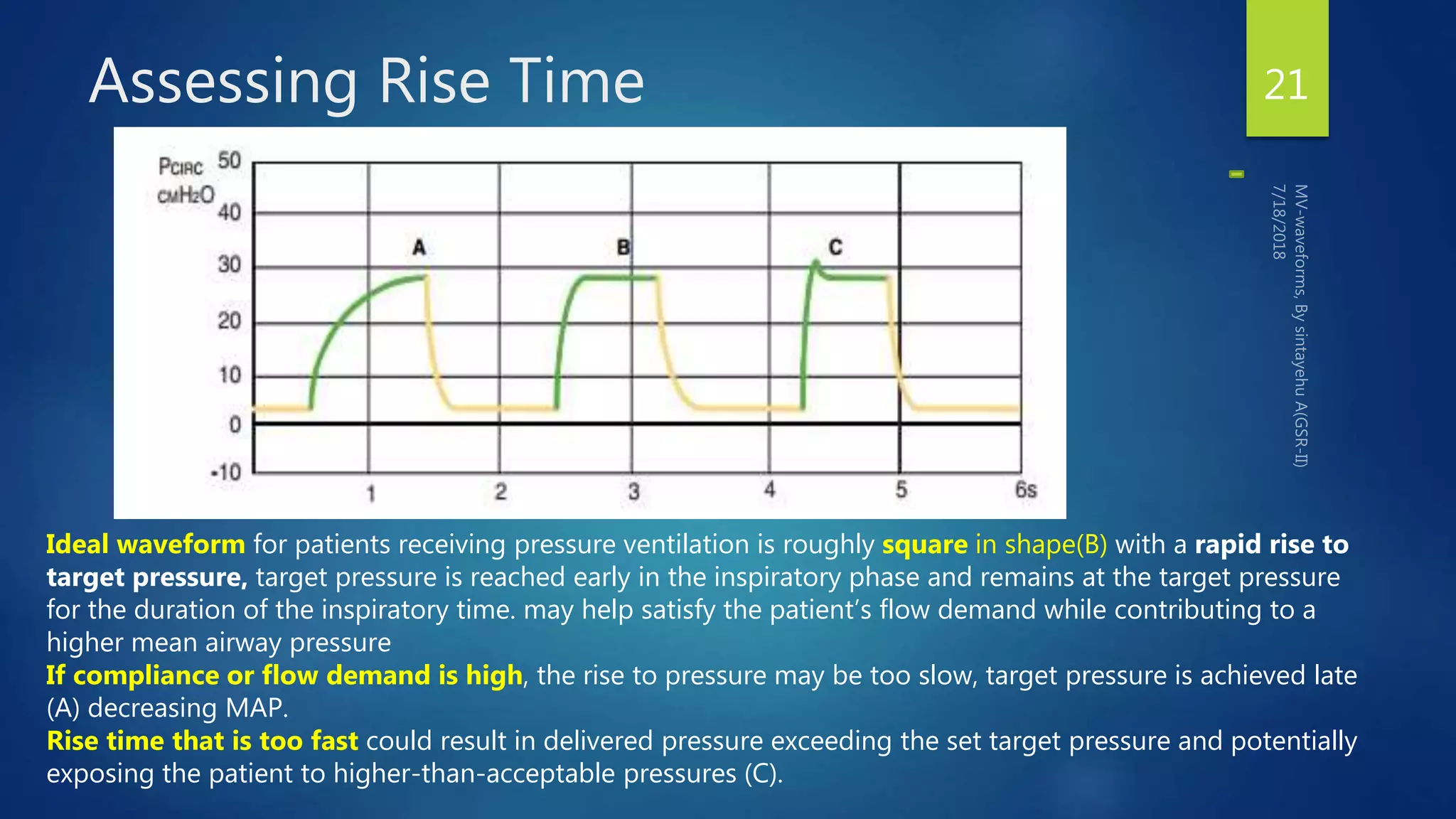
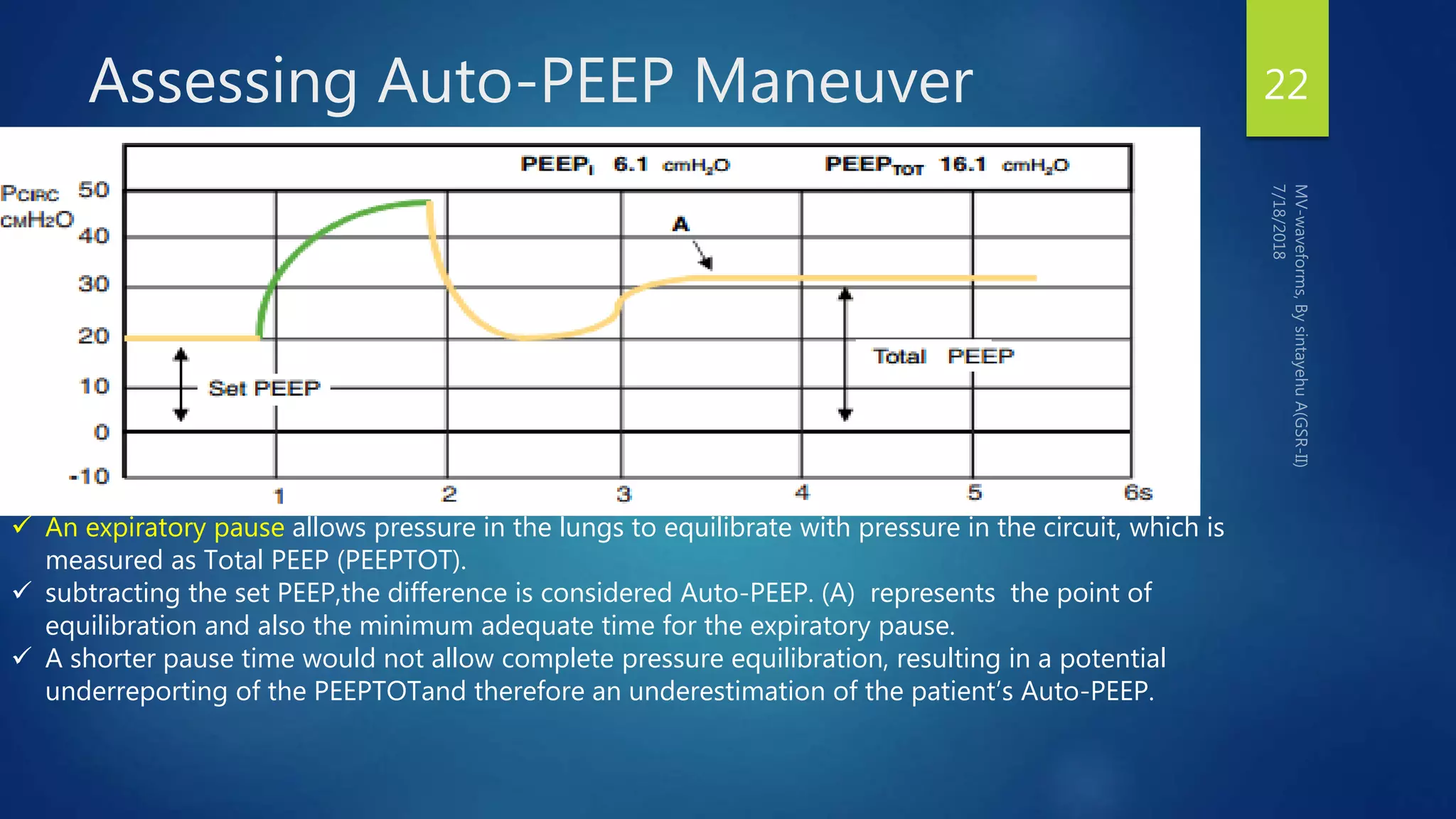
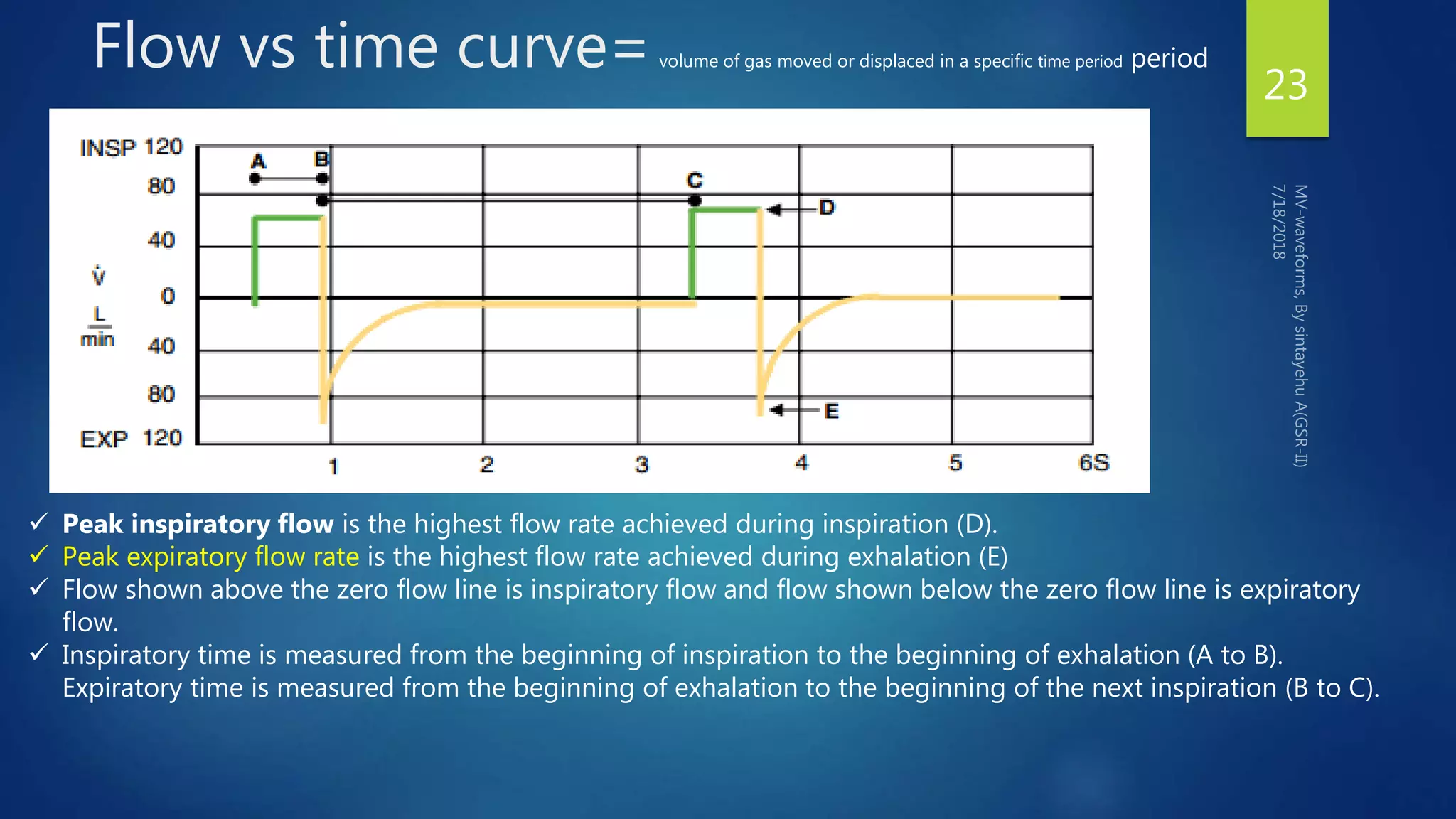
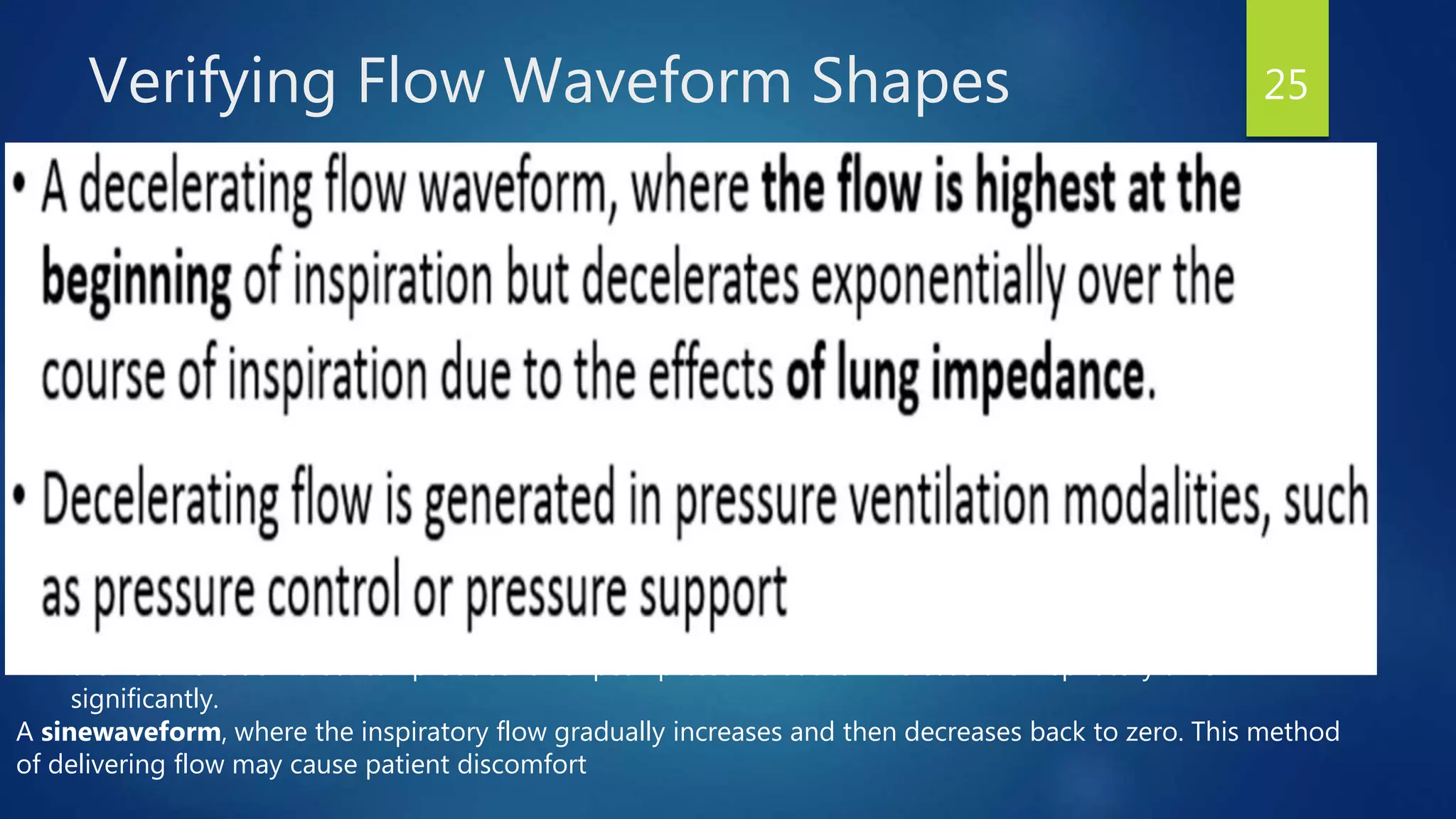
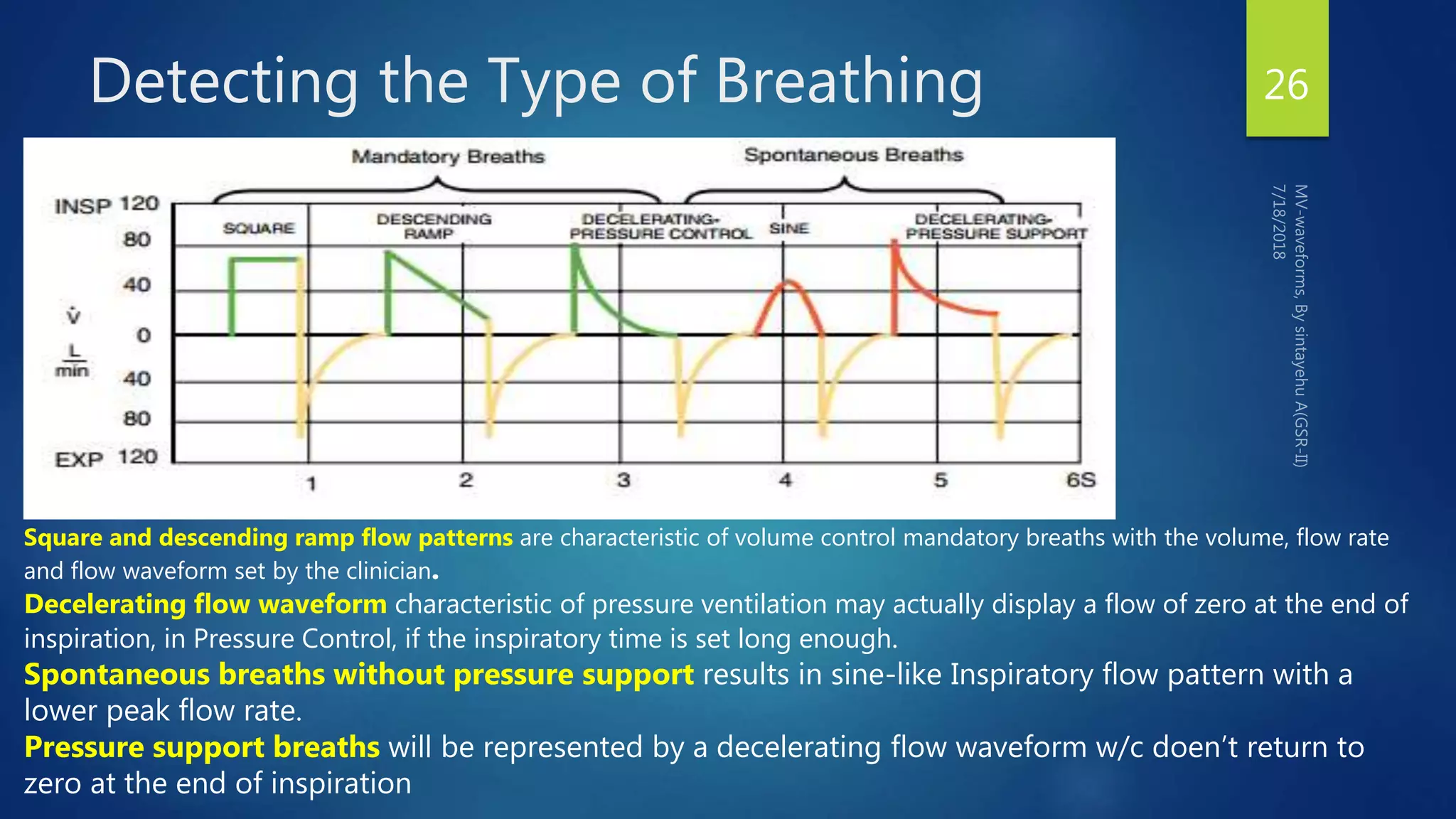
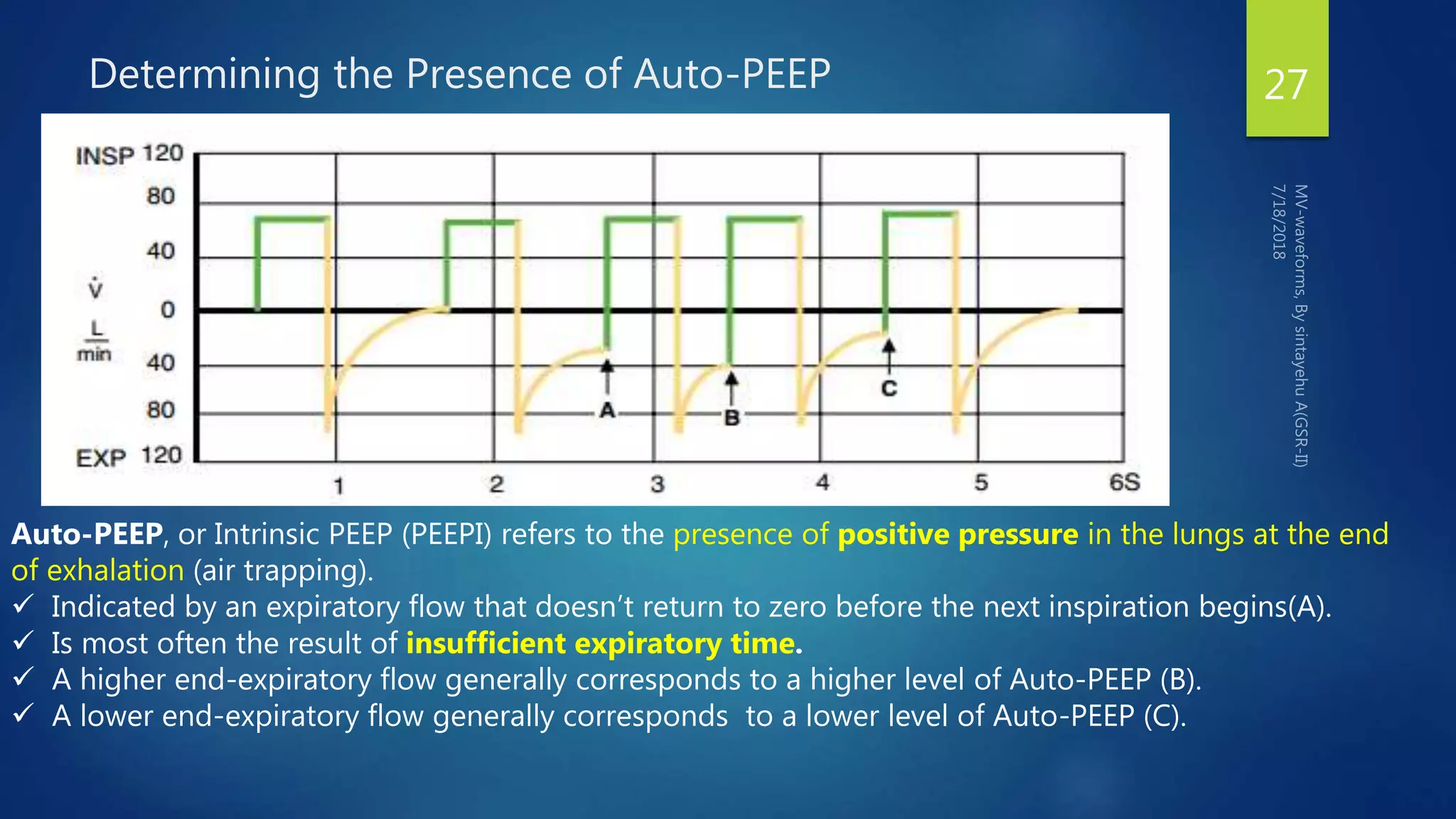
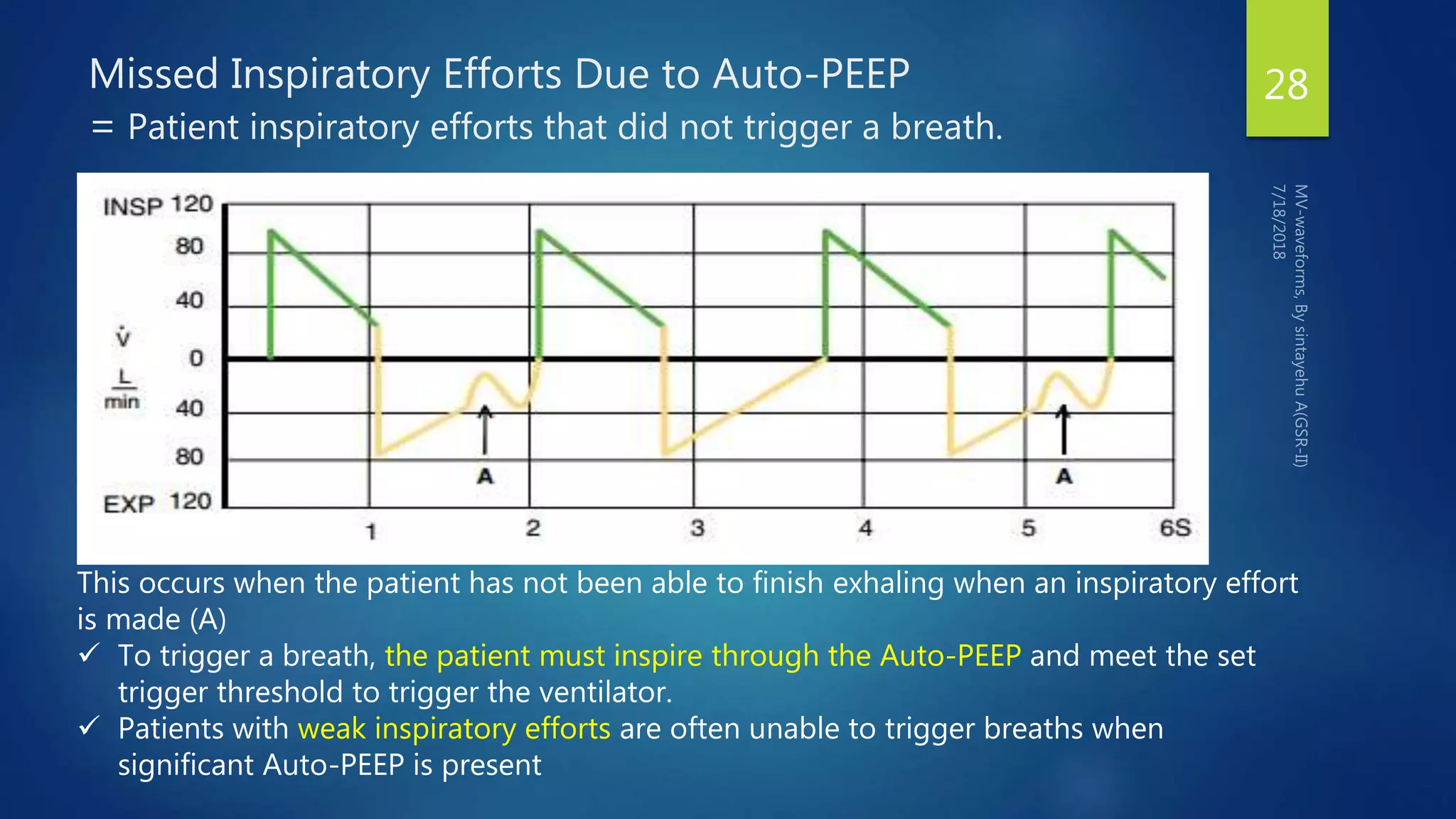
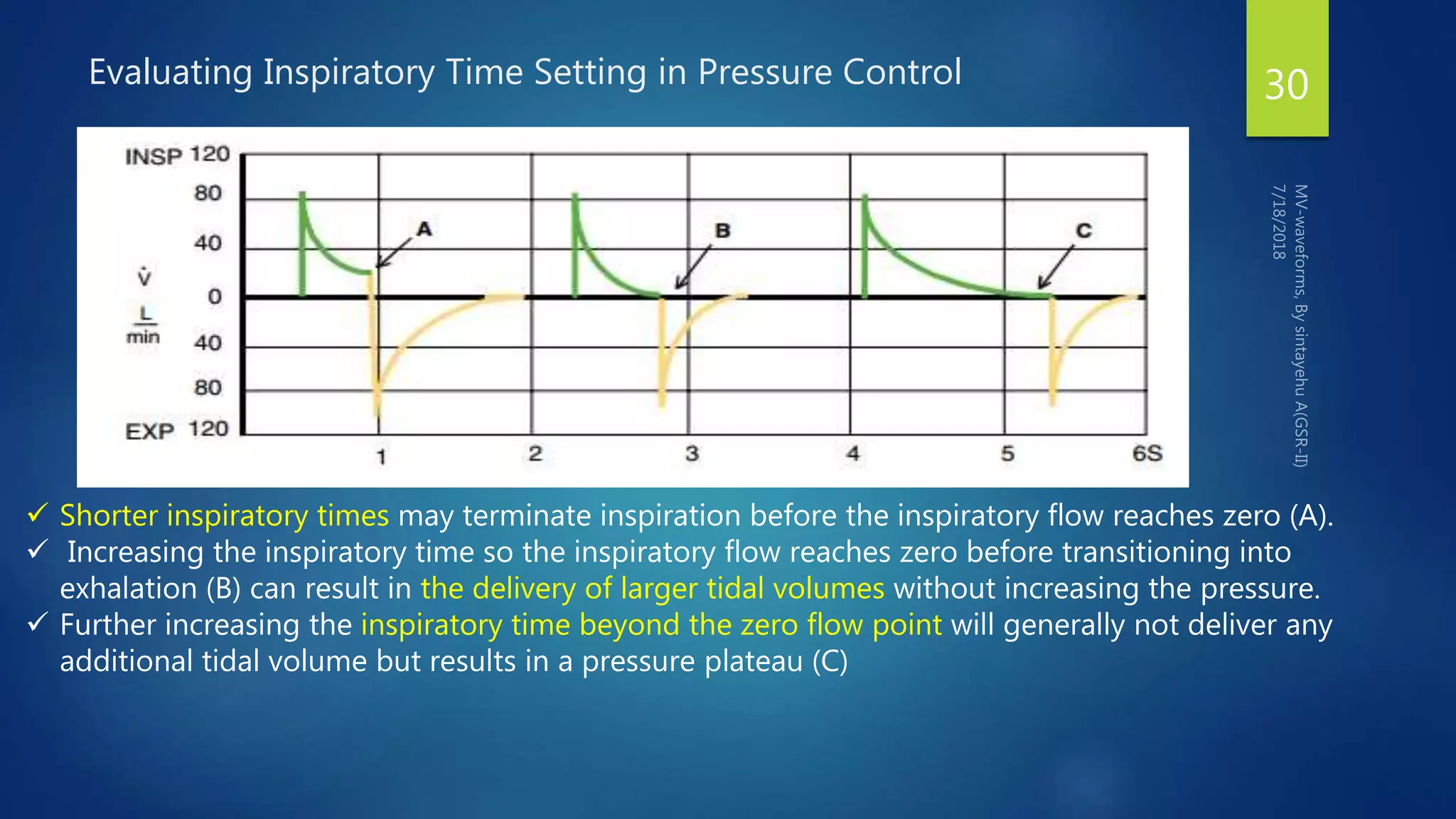
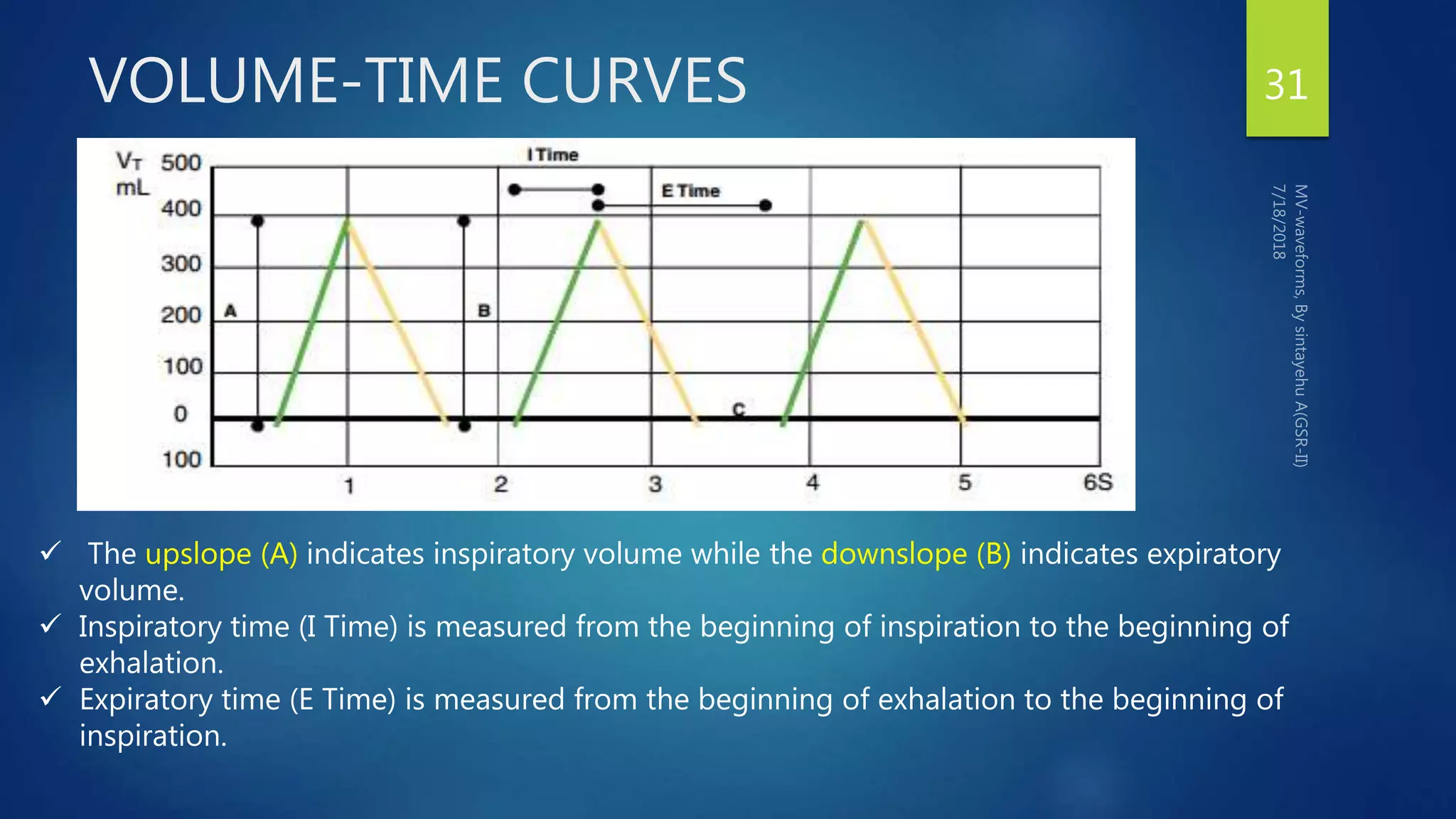
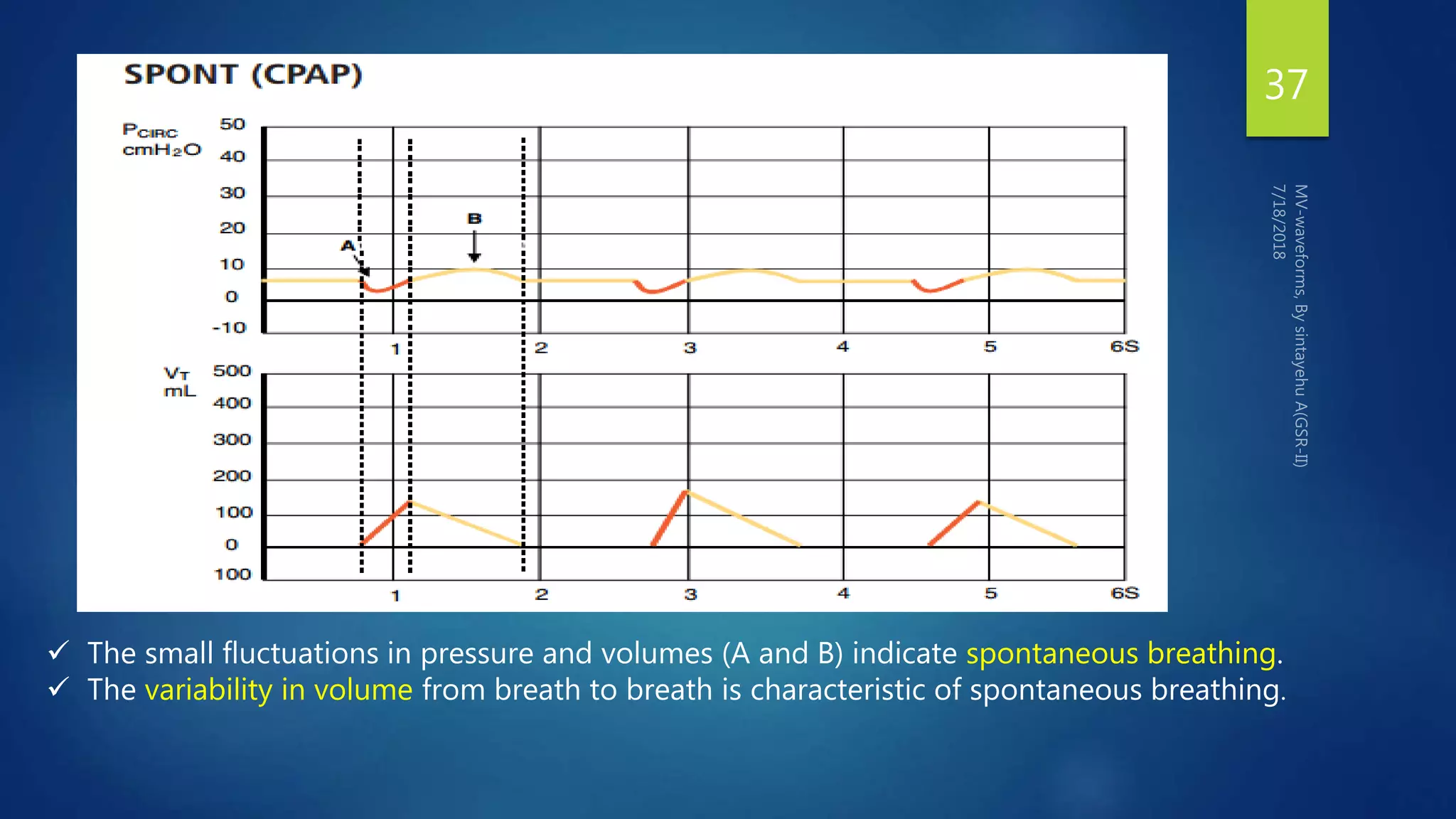
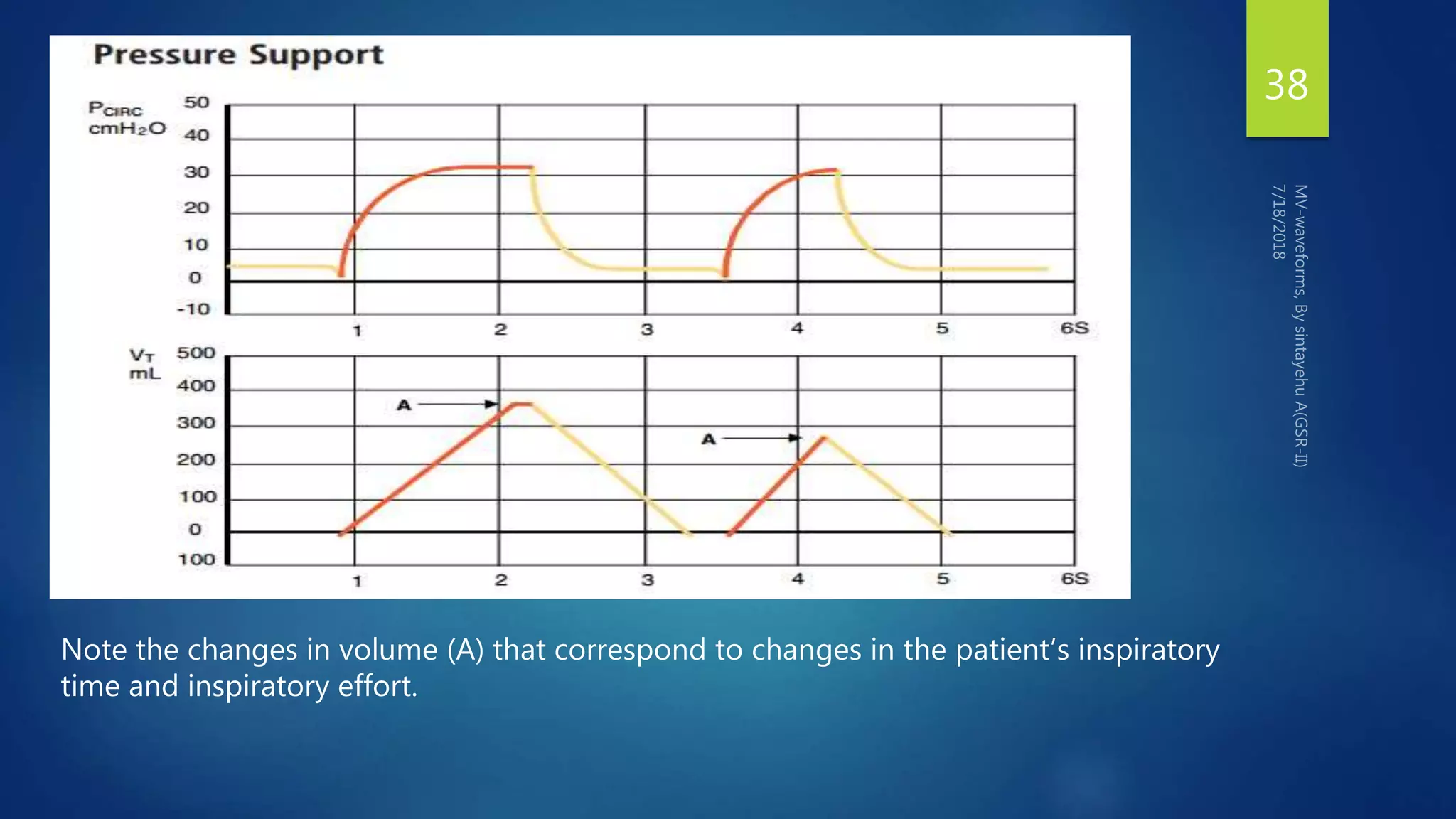
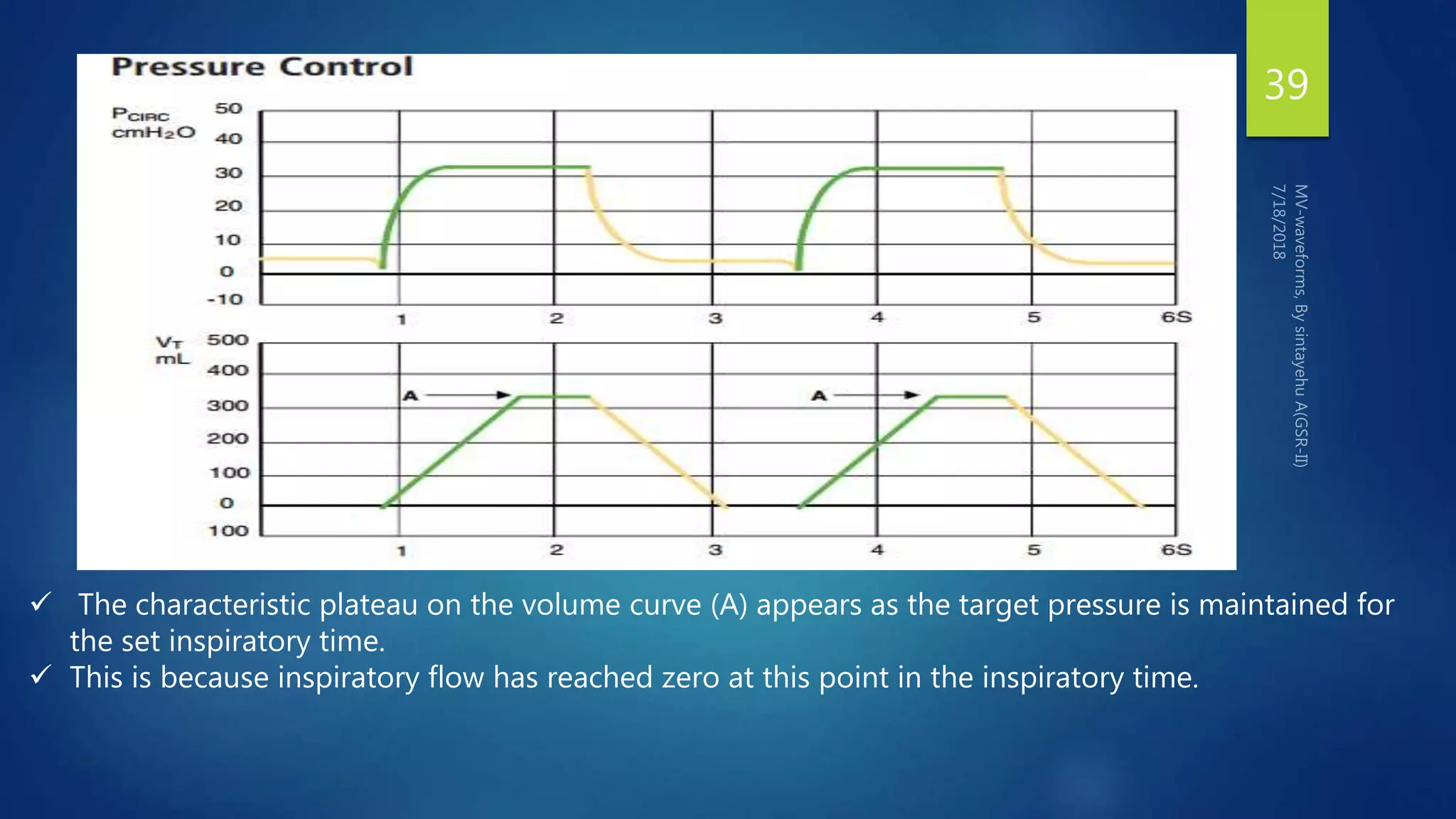
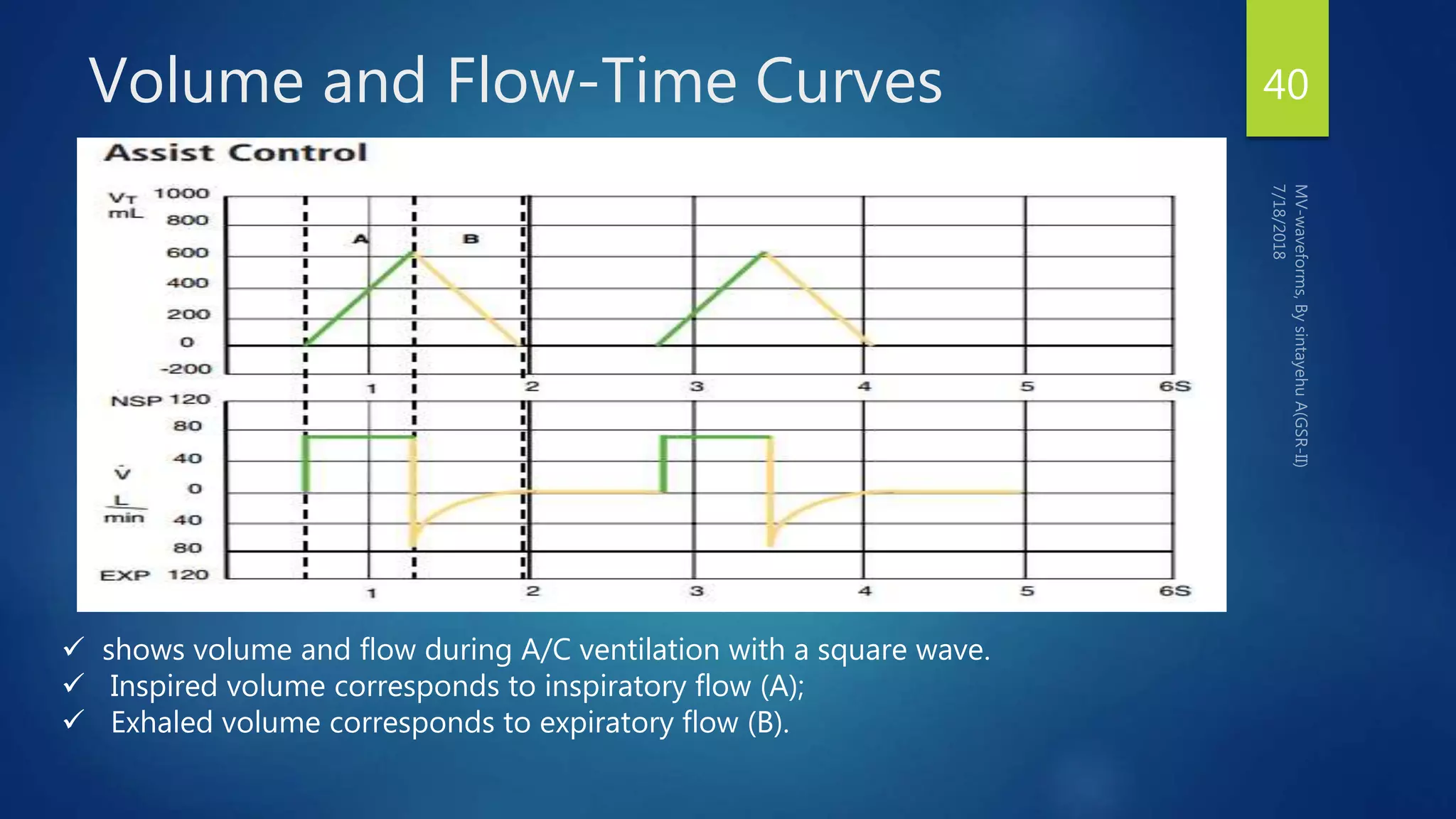
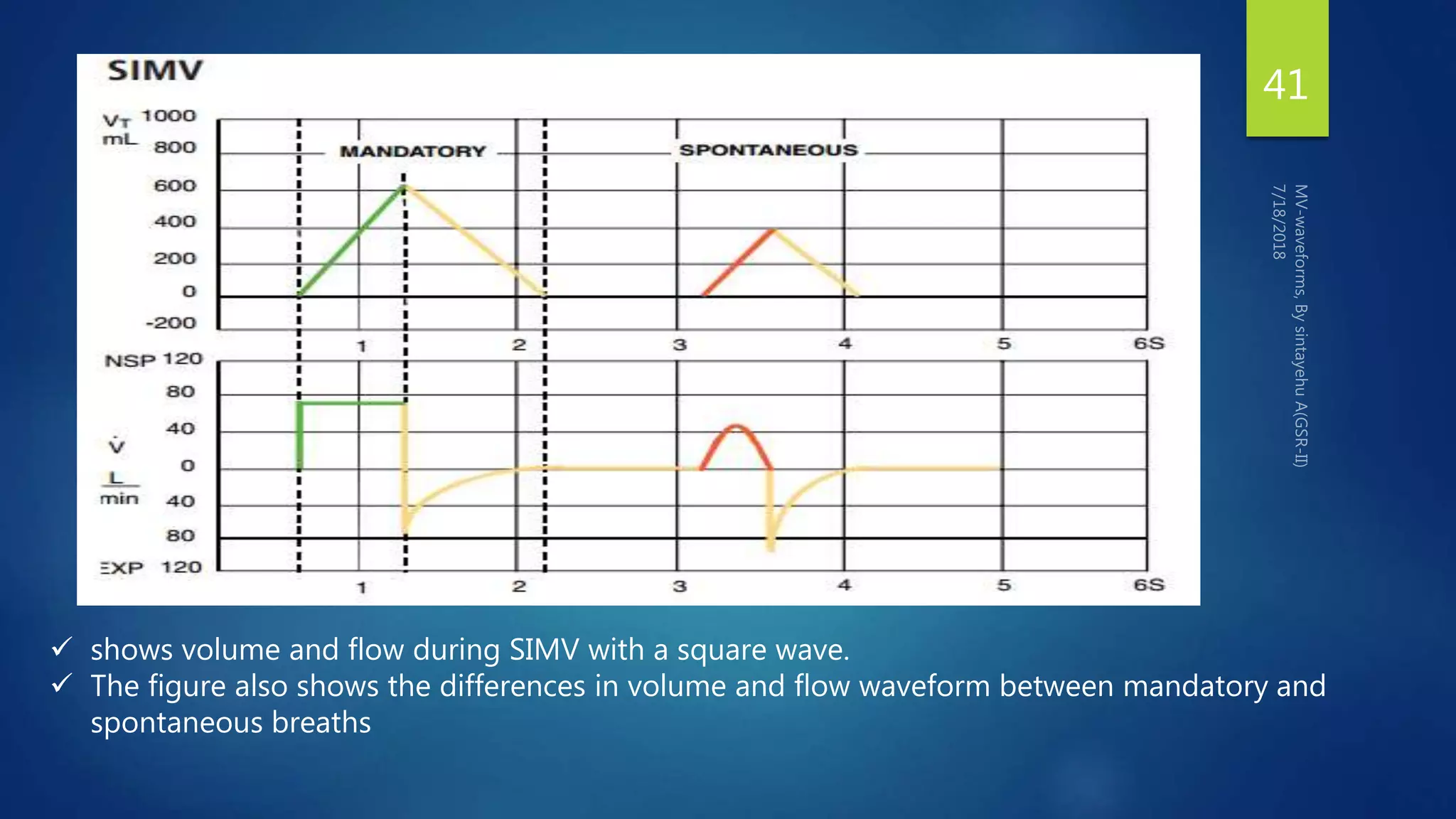
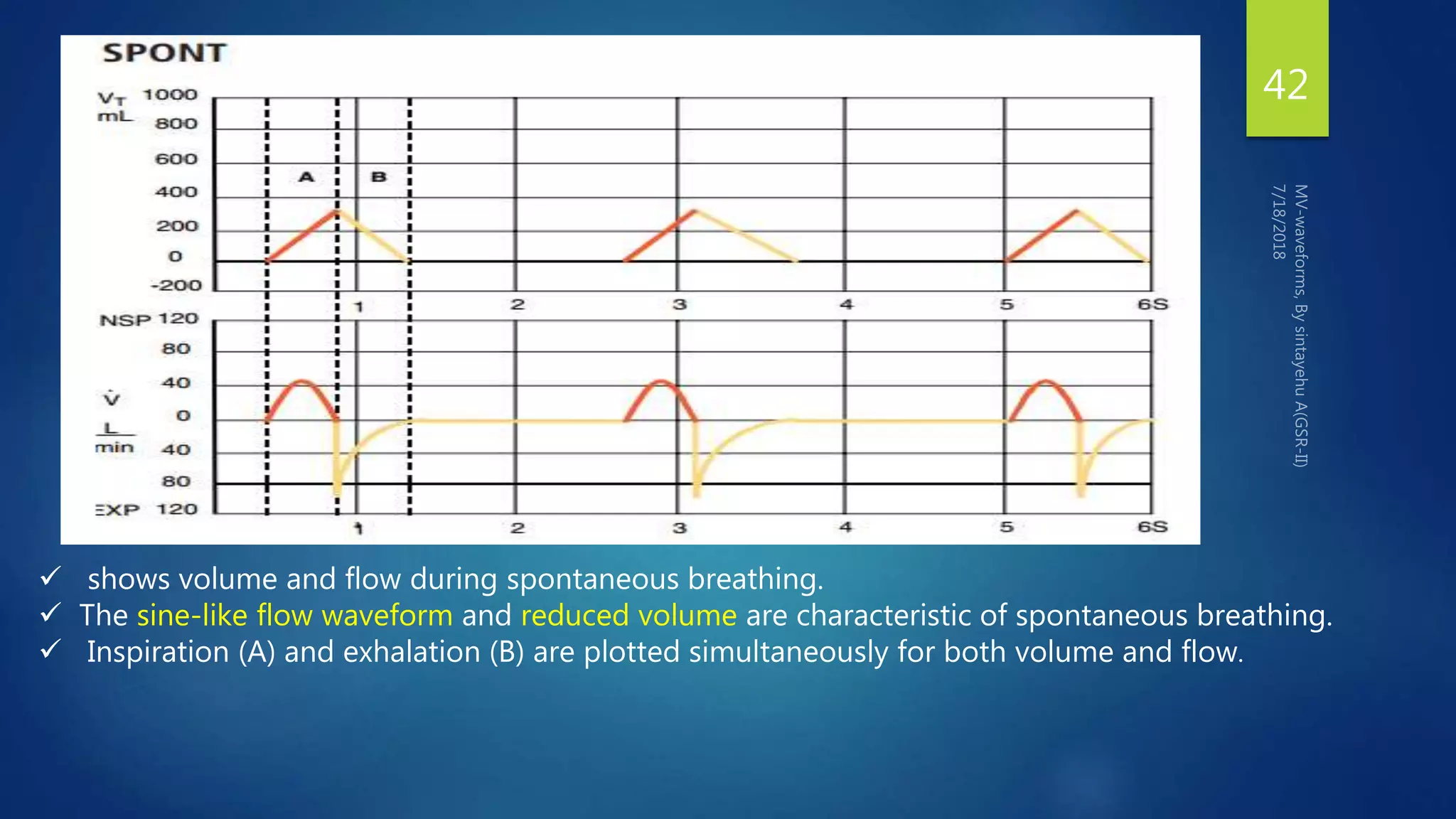
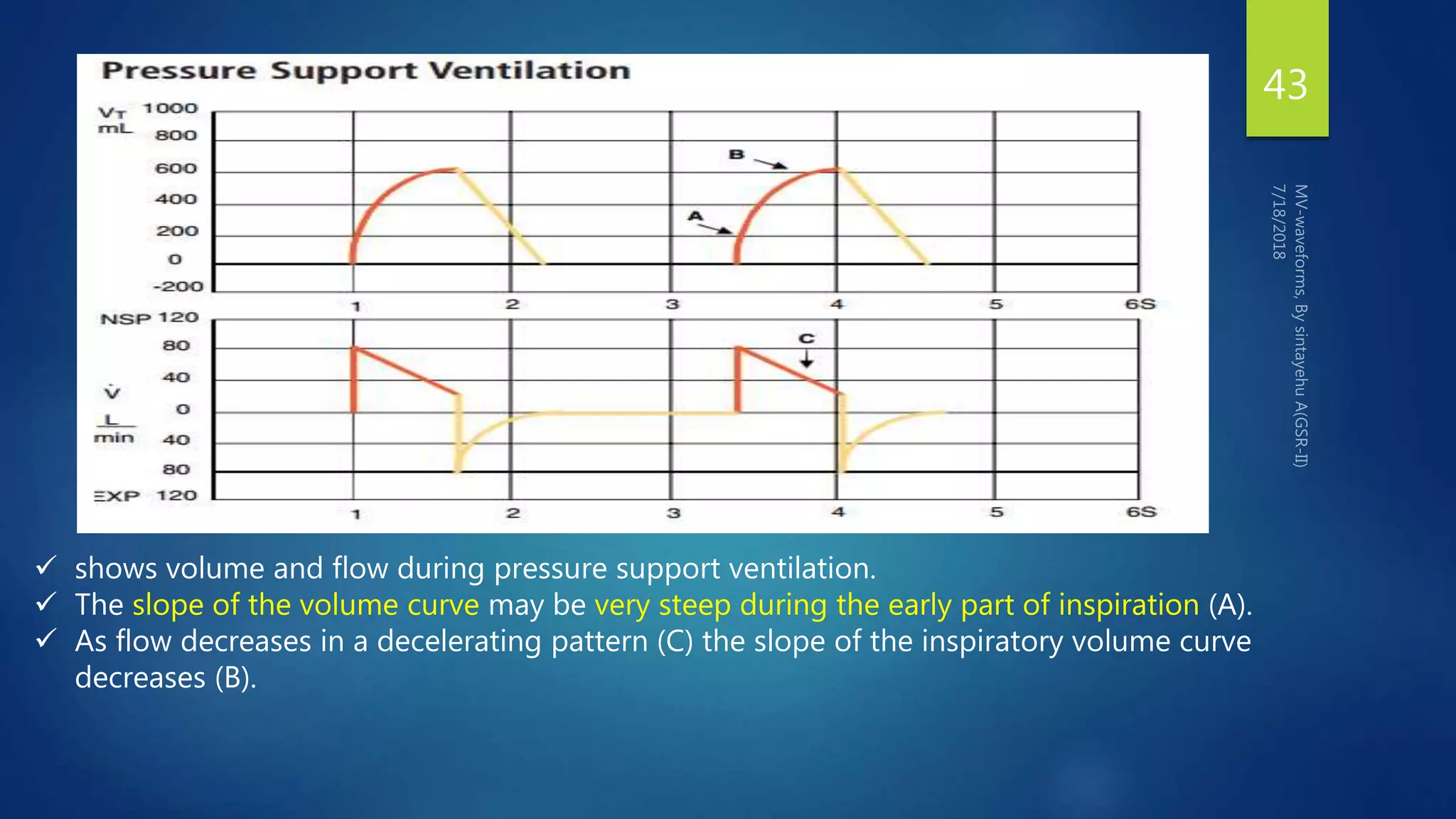
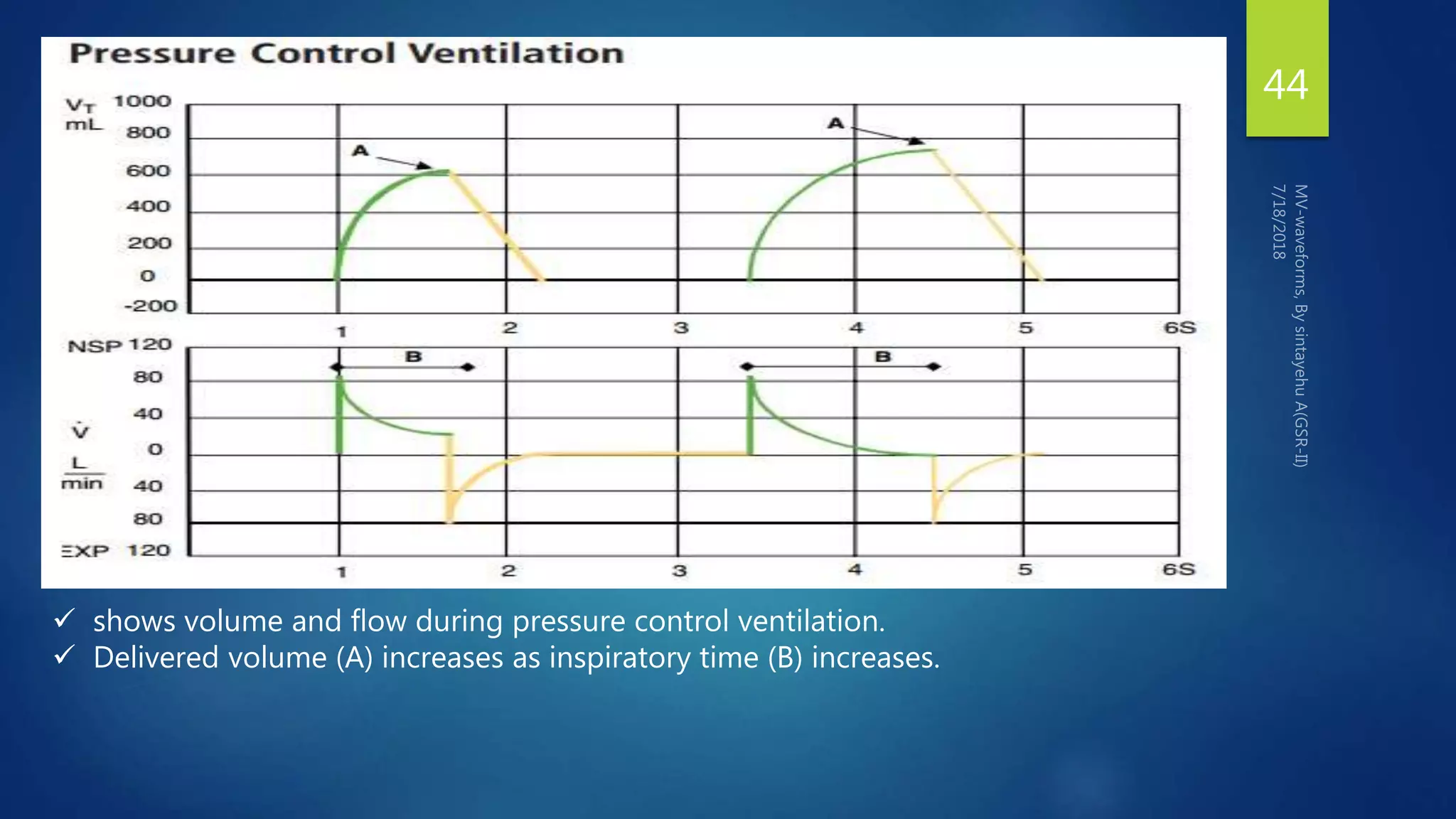
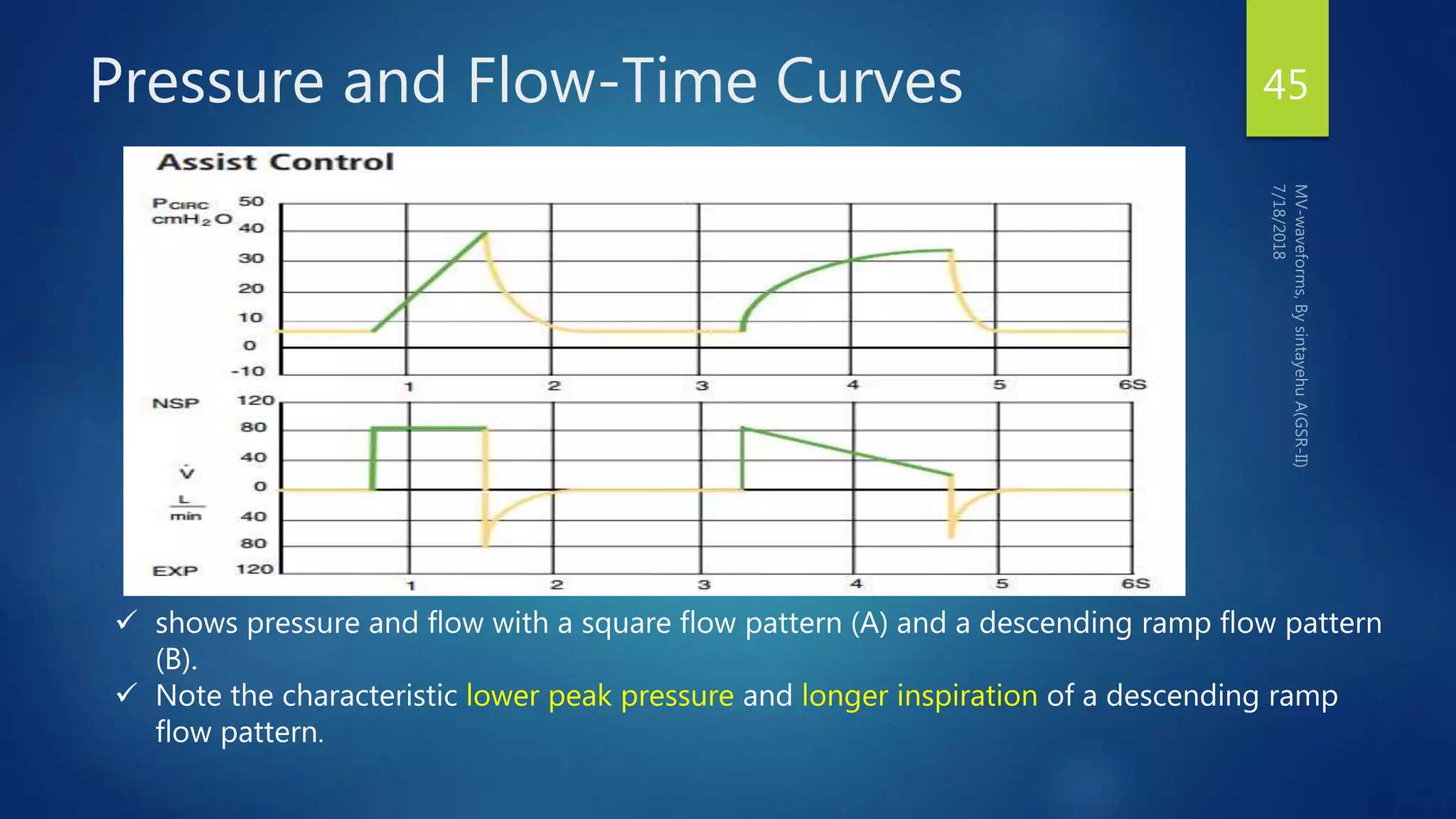
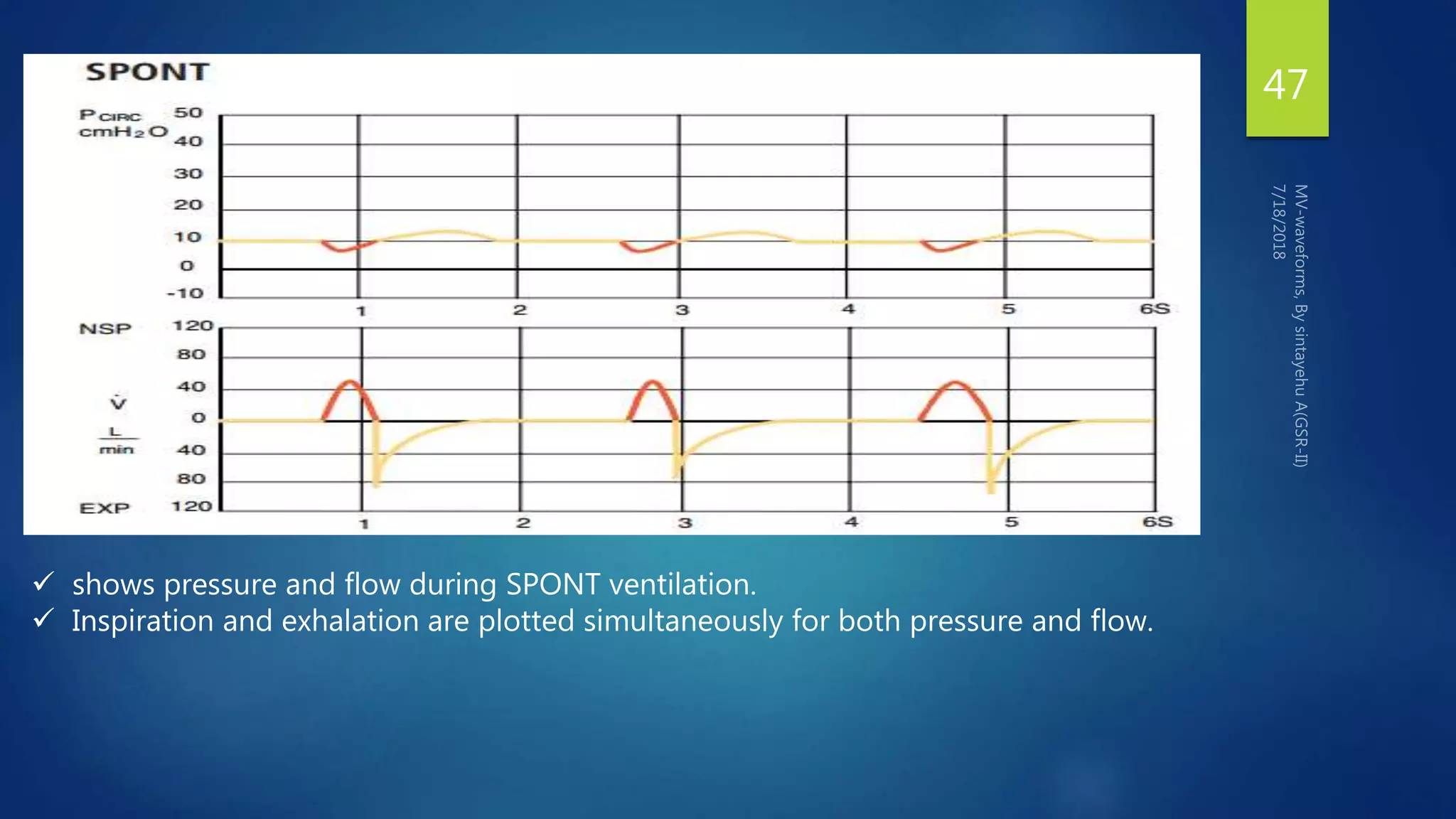
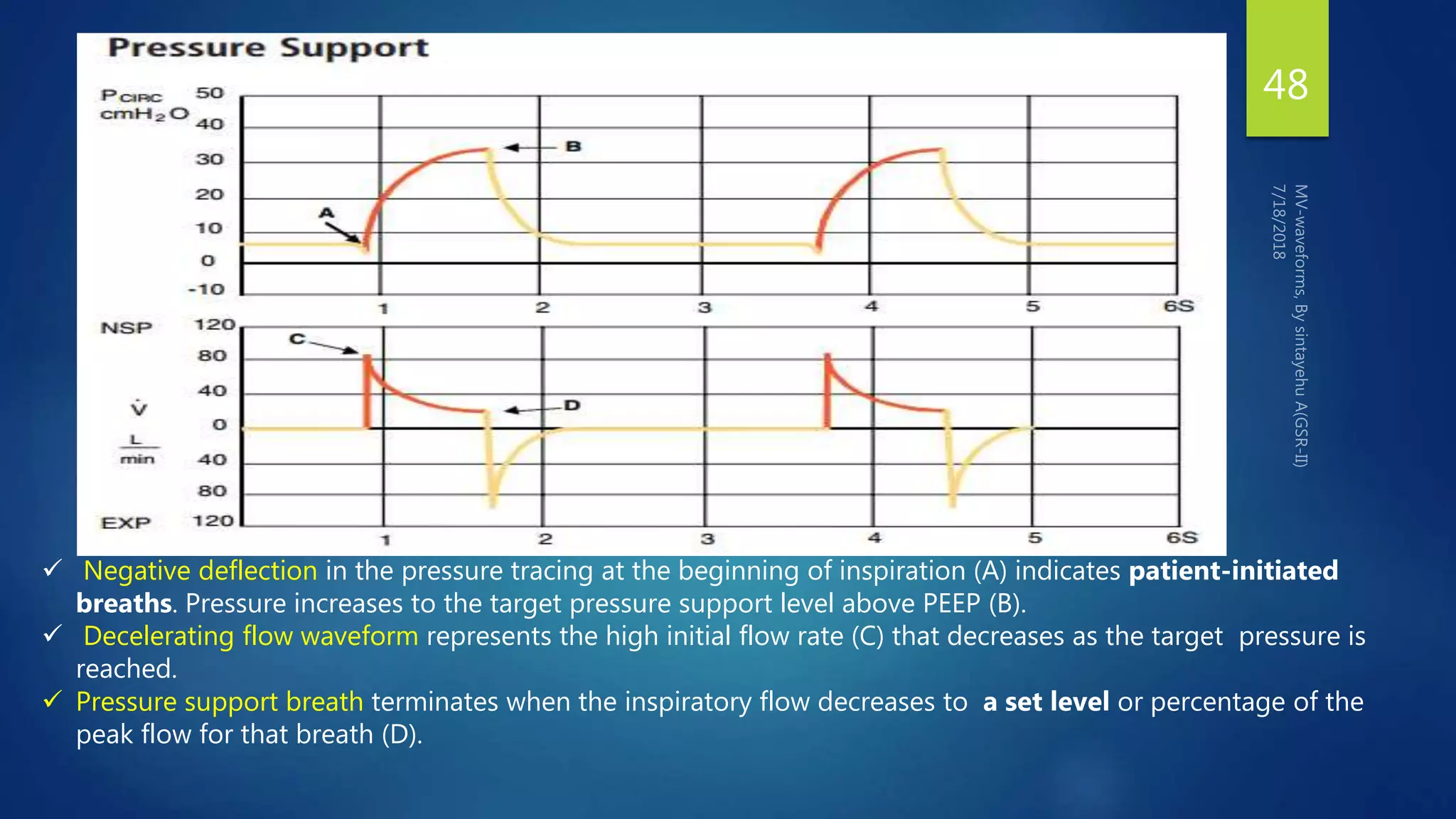
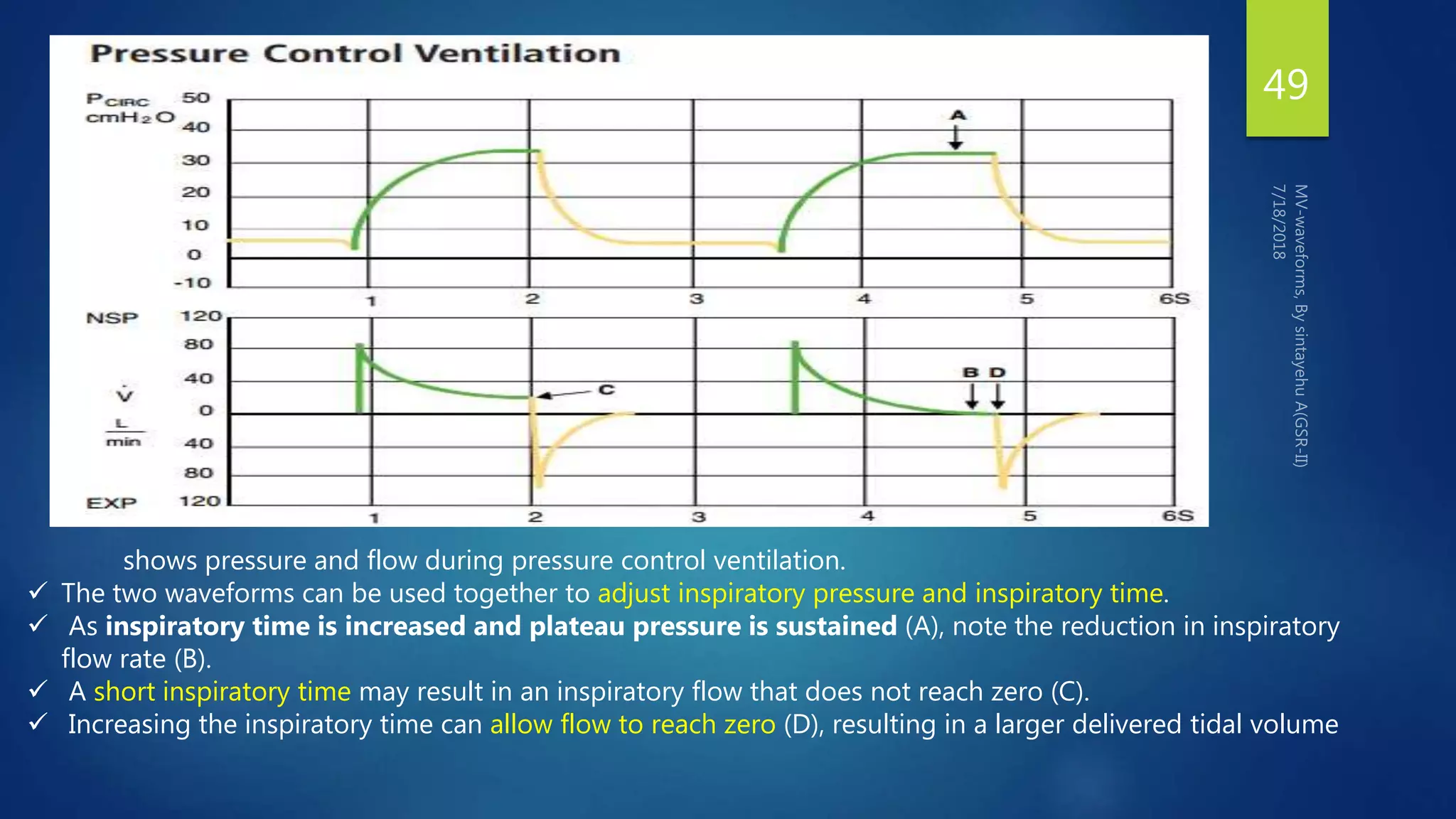
This document discusses mechanical ventilation waveforms. It begins by stating the objectives are to discuss commonly used waveforms, their applications, and combined waveforms. It then provides an outline and introduction on waveforms and how they represent ventilator data graphically over time or against each other. The majority of the document discusses specific commonly used waveforms including pressure-time, flow-time, and volume-time curves and how to interpret each to evaluate the patient and ventilator settings.