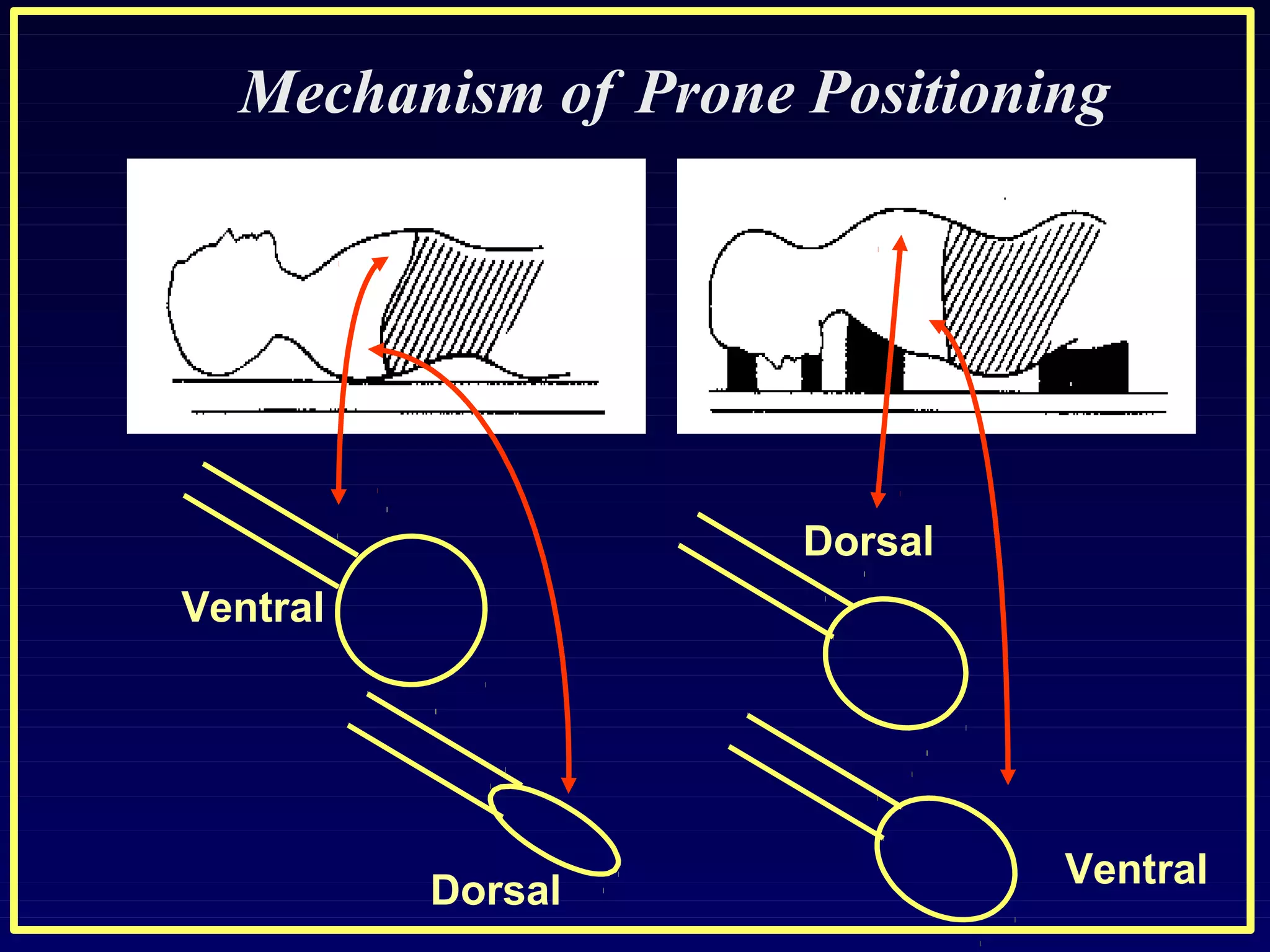
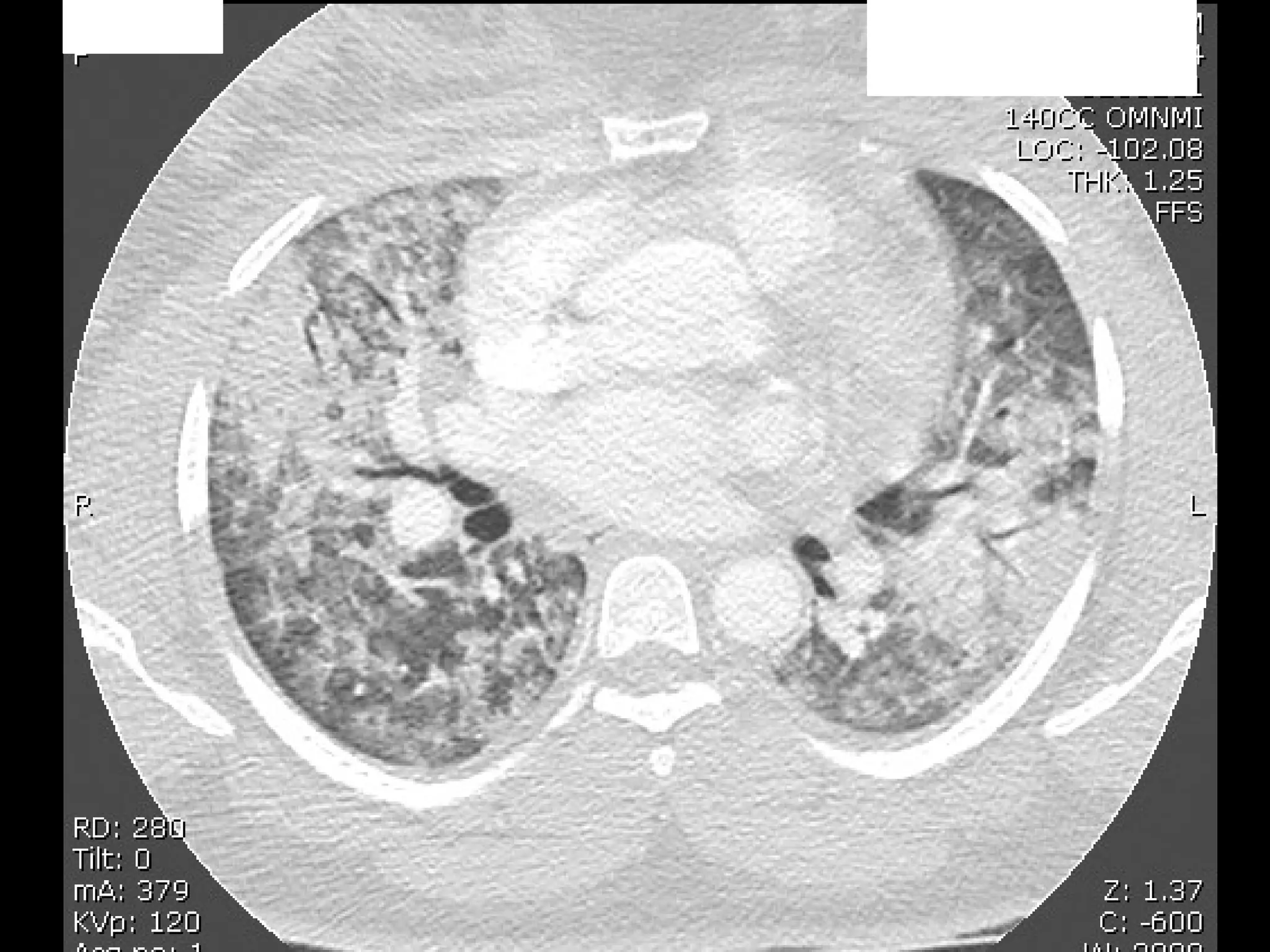
The document discusses the case of a 27-year-old postpartum woman presenting with worsening dyspnea and hypoxia. It then reviews the key considerations and management strategies for acute respiratory distress syndrome (ARDS), including low tidal volume ventilation, open lung strategies using recruitment maneuvers and high positive end-expiratory pressure, unconventional approaches like airway pressure release ventilation and high frequency oscillatory ventilation, and adjunctive therapies such as prone positioning. The optimal ventilator mode, settings, and adjunctive strategies depend on the individual patient's severity of lung injury and response to different interventions.










![Low tidal volume ventilation (LTVV)
Benefit
-The multicenter ARMA trial randomly assigned 861 mechanically
ventilated patients with ARDS to receive LTVV (initial tidal volume of 6
mL/kg predicted body weight [PBW]) or conventional mechanical
ventilation (initial tidal volume of 12 mL/kg PBW) .
The LTVV group had a lower mortality rate (31 versus 40 percent) and
more ventilator-free days (12 versus 10 days).](https://image.slidesharecdn.com/ardsandventilatormanagement-180704084743/75/Ards-and-ventilator-management-18-2048.jpg)









![Mode of ventilation
- In order to adhere to a strategy of LTVV, it is probably
easier to use a volume limited approach. However, a pressure
limited mode is an acceptable alternative, as long as the
resulting tidal volumes are stable and consistent with the
strategy of LTVV.
-Regardless of whether volume limited or pressure limited
ventilation is chosen, fully supported modes of mechanical
ventilation (eg, assist control) are generally favored over
partially supported modes (eg, [SIMV]). This is particularly
true early in the course of disease.
-Ultimately, the choice of mode depends primarily on clinician
comfort and familiarity.](https://image.slidesharecdn.com/ardsandventilatormanagement-180704084743/75/Ards-and-ventilator-management-33-2048.jpg)