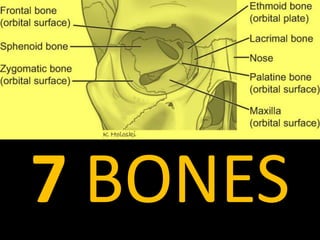
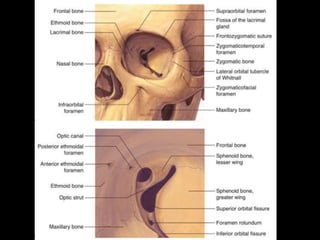
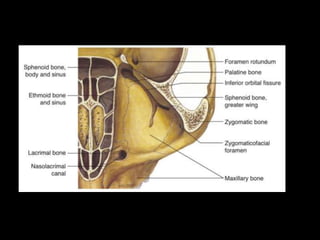
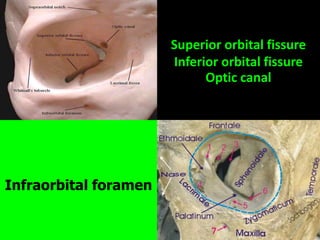
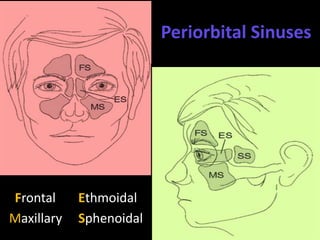
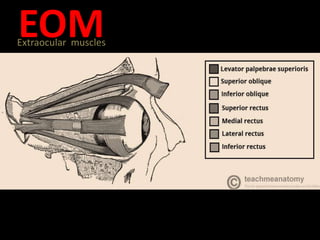
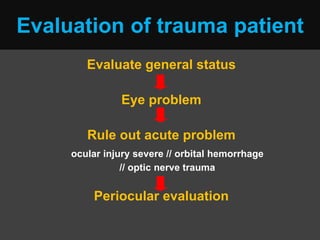
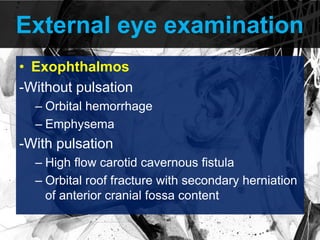
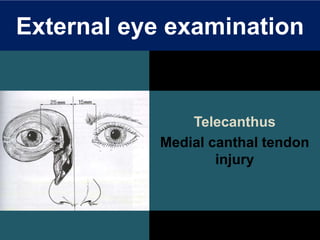
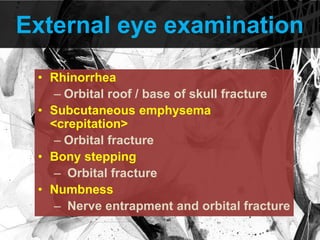
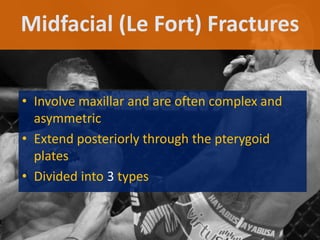
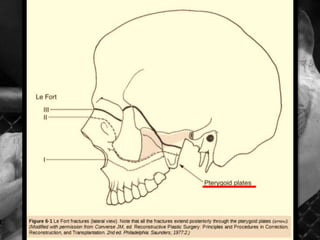
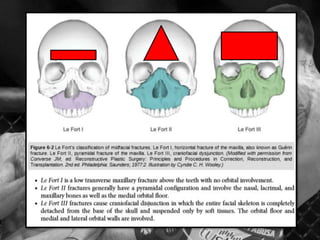
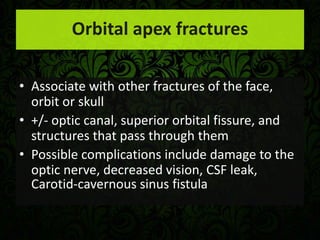
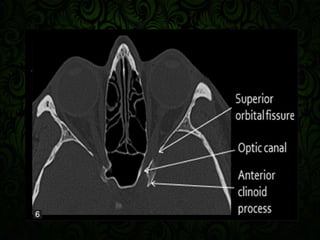
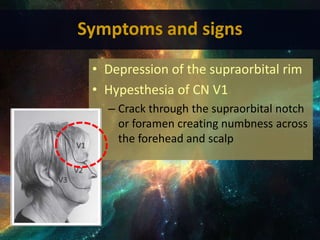
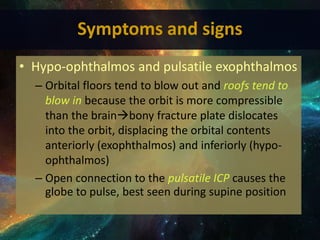
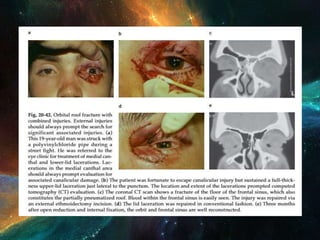
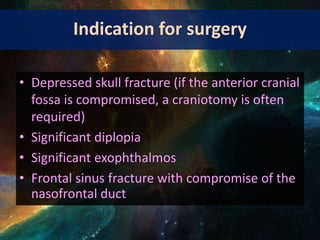
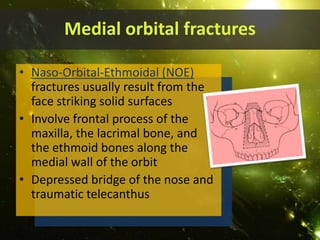
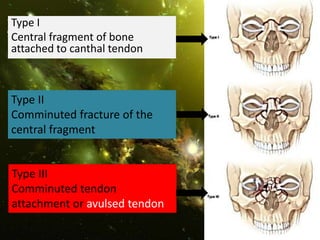
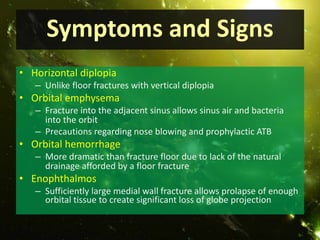
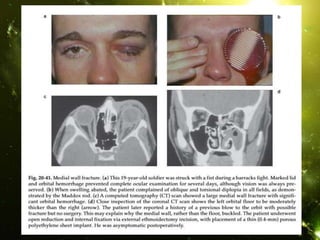
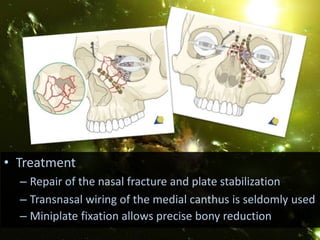
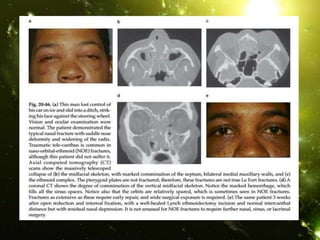
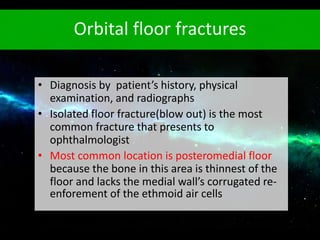
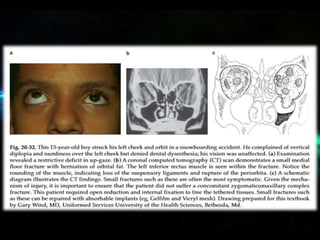
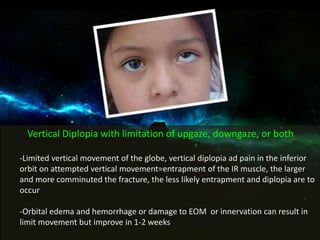
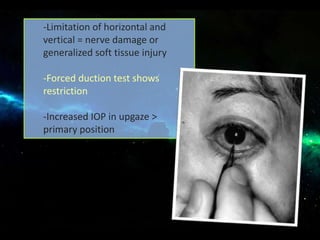
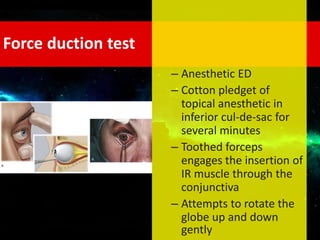
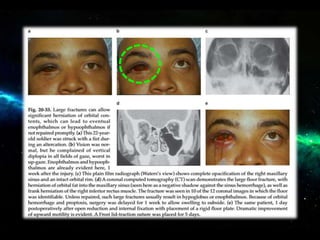
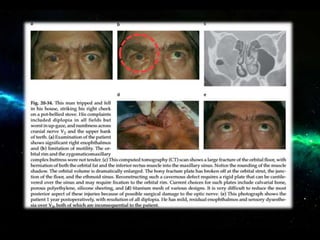
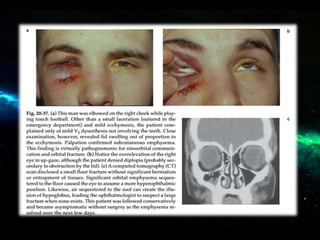
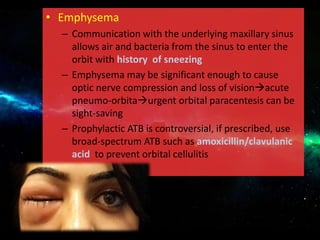
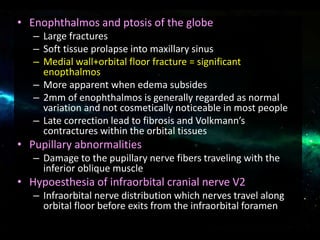
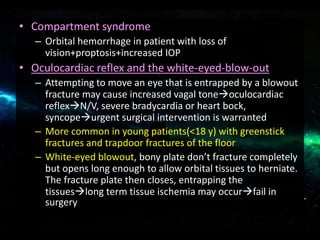
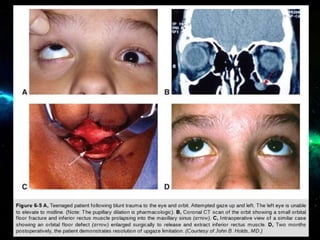
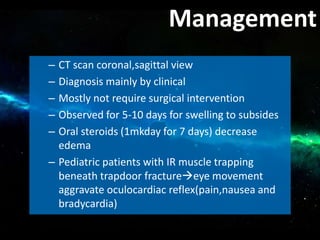
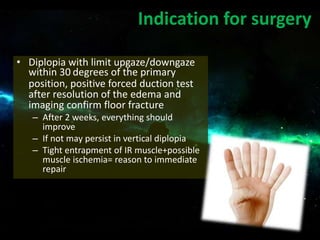
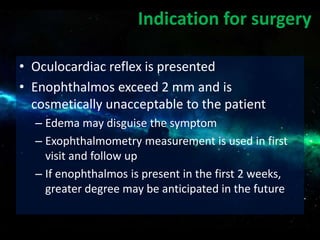
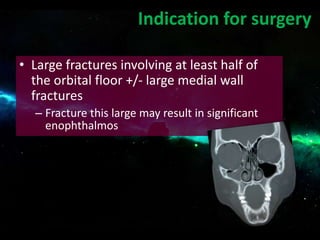
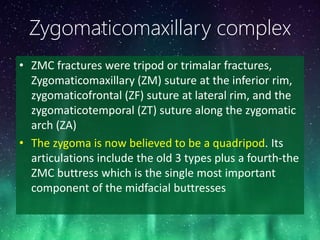
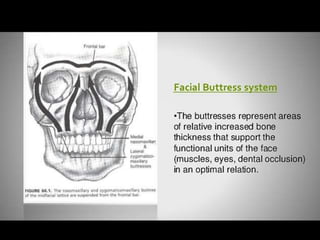
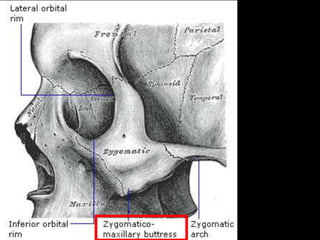
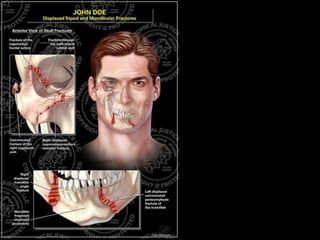
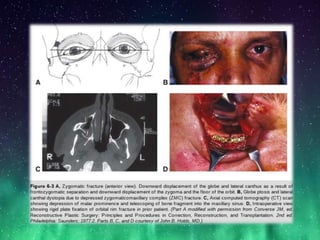
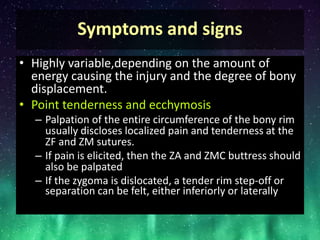
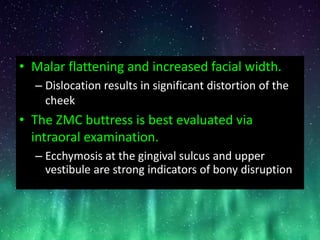
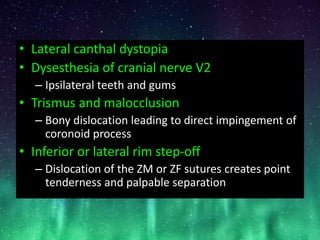
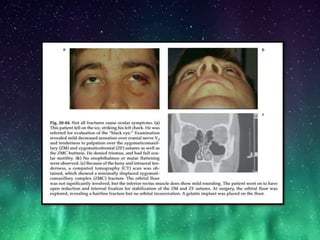
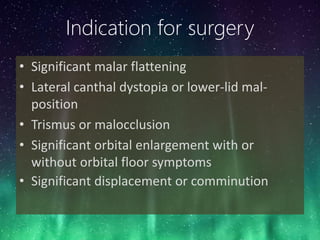
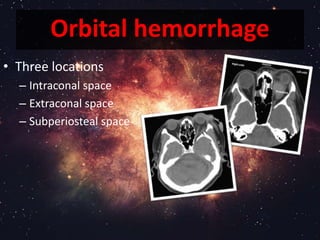
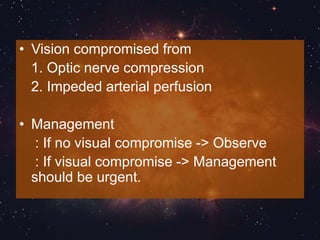
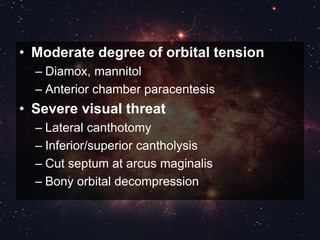
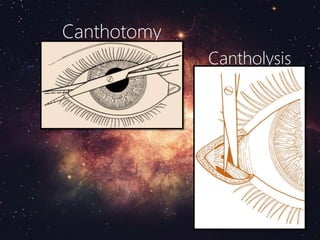
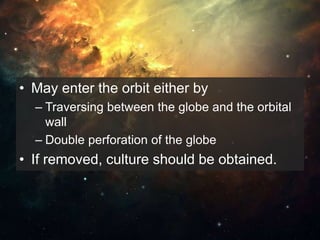
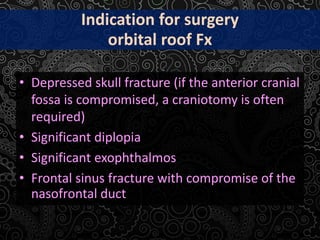
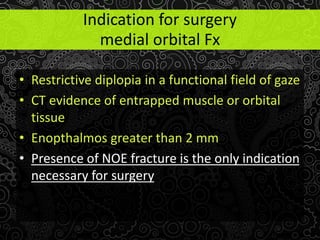
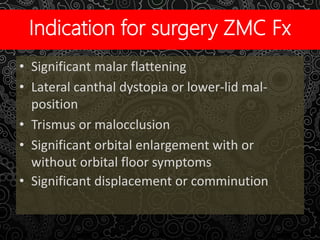
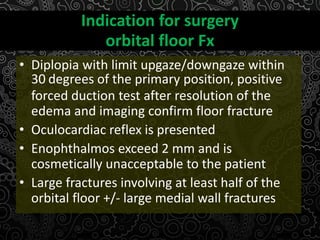
The document provides a comprehensive overview of orbital trauma, including its anatomy, types of injuries such as hemorrhages and fractures, and their associated symptoms and treatment indications. It highlights the complexities of midfacial fractures, evaluates symptoms based on physical examination, and discusses surgical intervention criteria based on complications like significant diplopia or enophthalmos. Overall, it serves as a guide for the assessment and management of orbital injuries in ophthalmology.