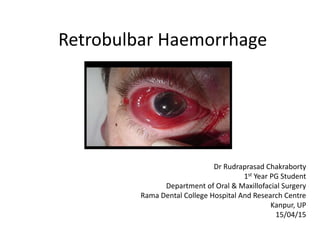
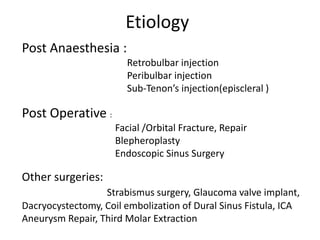
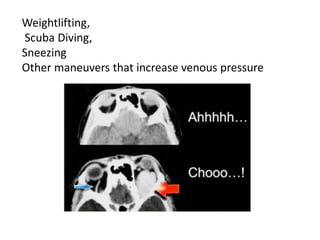
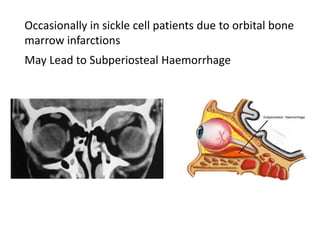
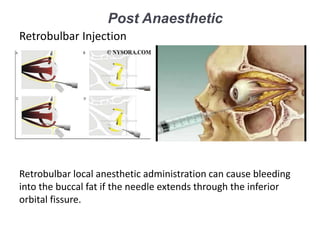
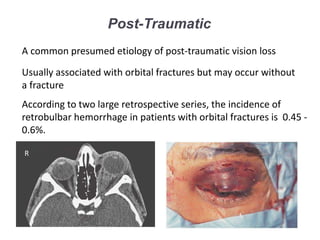
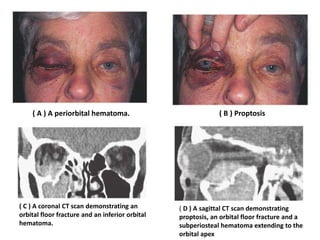
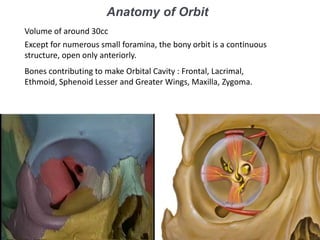
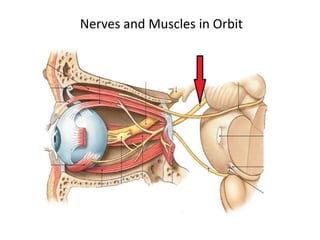
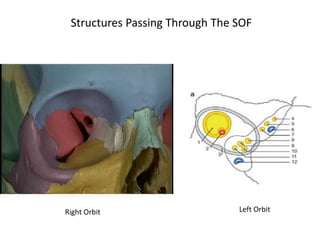
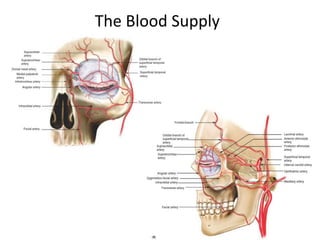
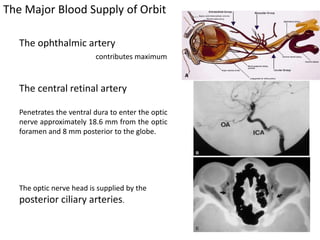
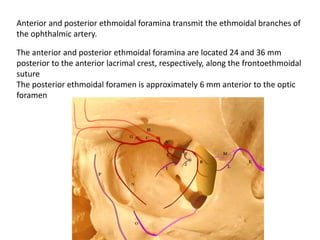
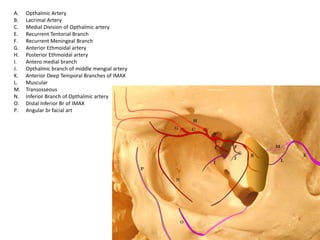
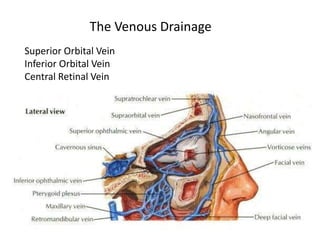
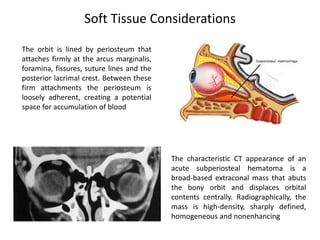
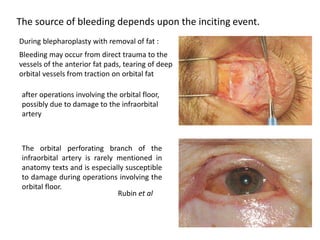
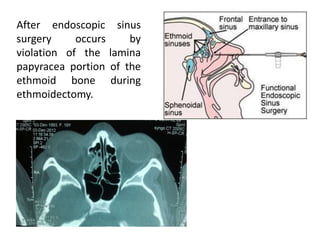
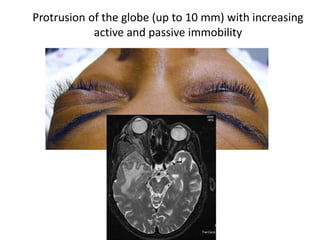
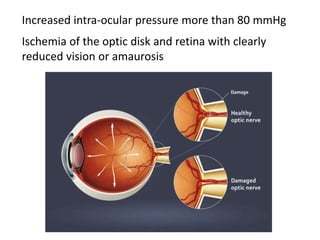
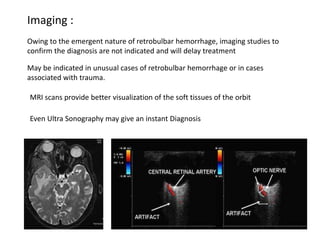
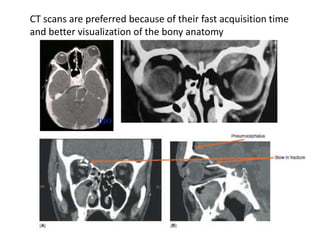
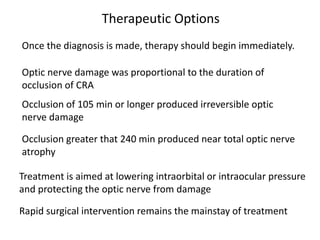
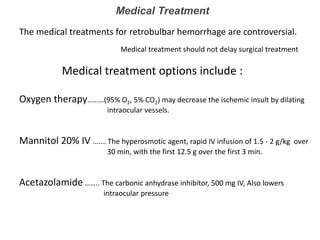
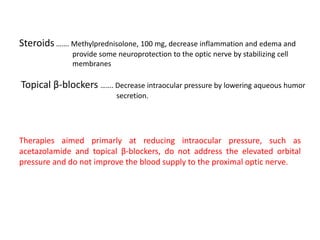
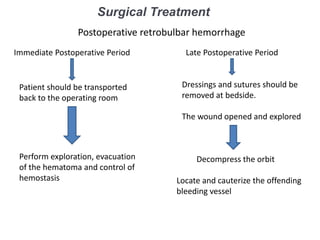
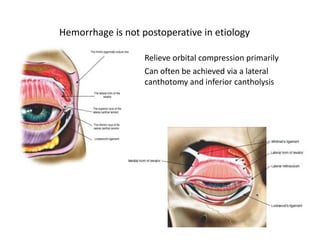
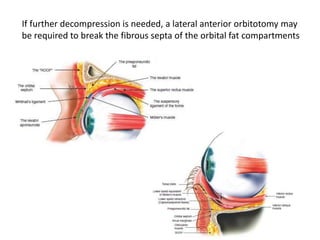
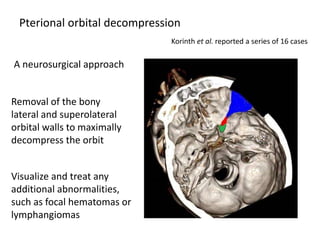
This document discusses retrobulbar hemorrhage, its causes, and clinical features, emphasizing the impact of increased intraorbital pressure and the risk of optic nerve damage. It outlines various etiologies including spontaneous cases, traumatic incidents, and complications from surgical procedures, as well as diagnostic imaging considerations. Treatment options, both medical and surgical, are reviewed, highlighting the urgency of intervention to preserve vision and reduce intraocular pressure.