This document provides an overview of ocular trauma, including classifications, signs, symptoms, and management approaches. It discusses various types of trauma such as blunt trauma, penetrating trauma, chemical injuries, and orbital fractures. Key points include:
- Ocular trauma can be caused by physical injury, chemicals, heat, or radiation. It is a leading cause of monocular blindness.
- Trauma is classified based on etiology (accidental, self-inflicted, occupational) and nature (physical, chemical, thermal, radiation). Physical trauma includes perforating, non-perforating, and blunt injuries.
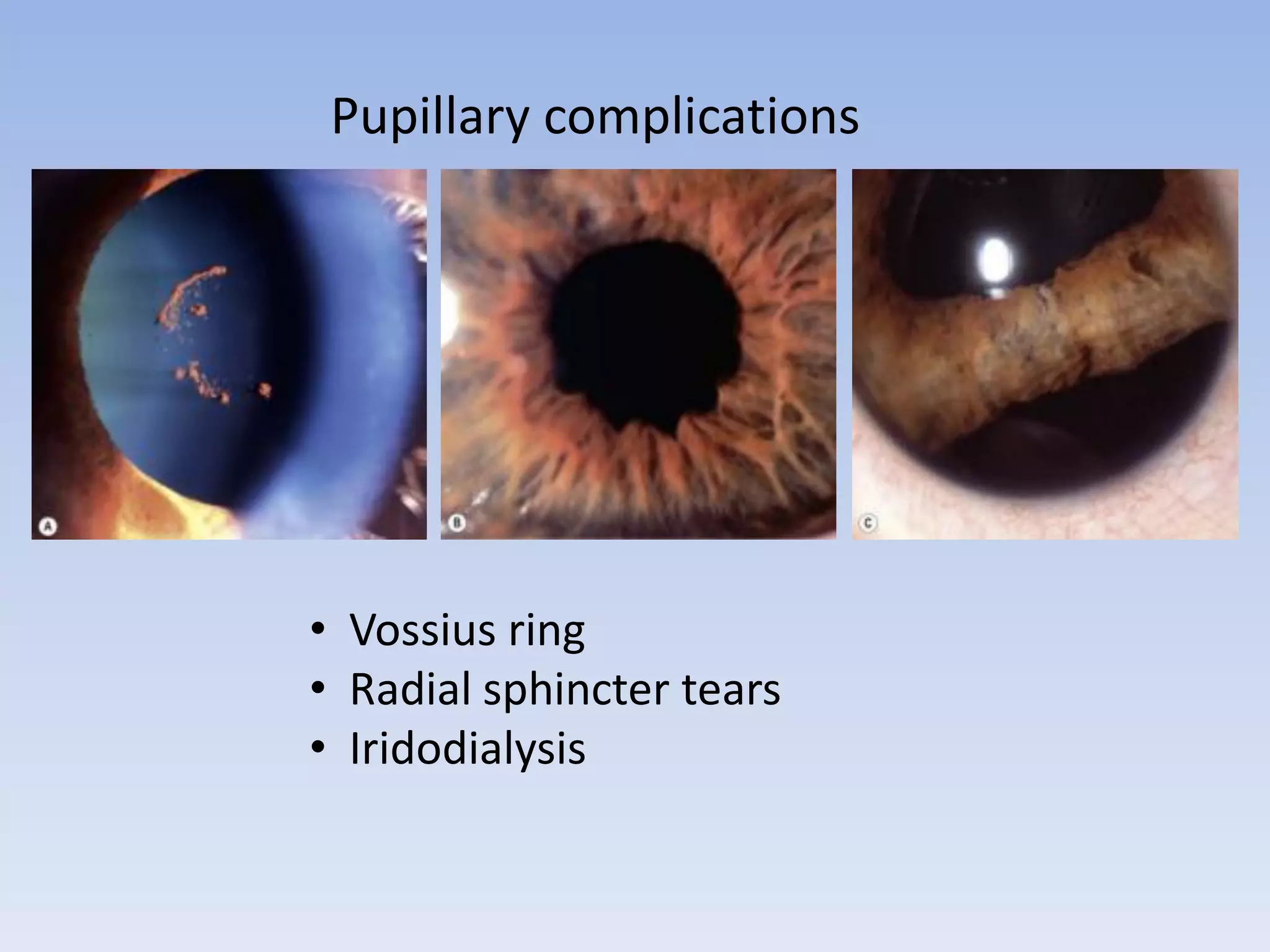
- Complications depend on the type and location of trauma but can include corneal abrasions,