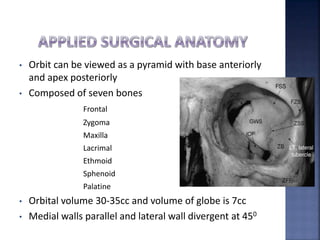
1) The document discusses the anatomy of the orbit and orbital fractures. It describes the bones that make up the orbit, the muscles, nerves, vessels and contents of the orbit.
2) It then focuses on orbital fractures, specifically enophthalmos and hypoglobus. It defines these conditions, lists their causes and signs, and describes methods for evaluation and surgical correction.
3) Surgical correction involves restoring the orbital volume and anatomy by reconstructing fracture sites with grafts or plates while also addressing issues like muscle dysfunction and scarring. The goals are to improve vision, eye movement and esthetics.