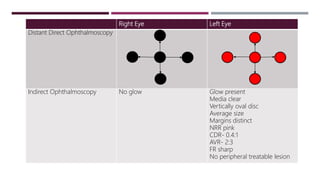
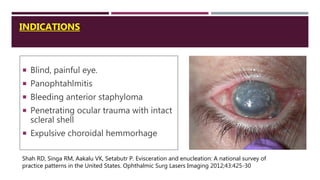
1. The document describes a case of a 73-year-old man who presented with spontaneous bleeding from his right eye along with pain and redness. He had a history of blindness in the right eye for 10 years along with glaucoma in both eyes.
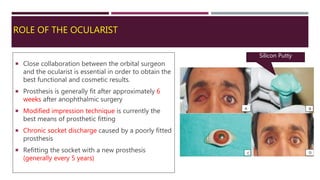
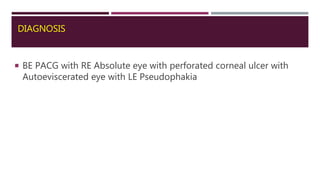
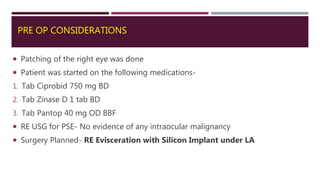
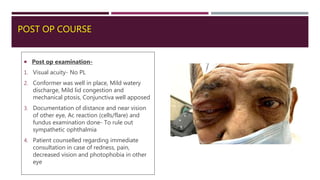
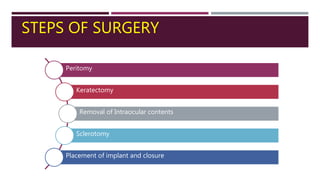
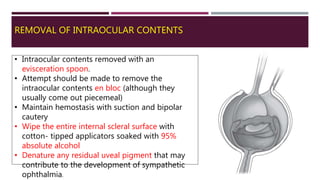
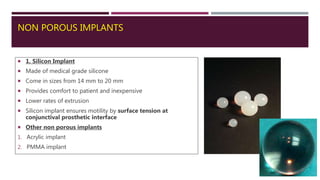
2. The patient underwent an evisceration of the right eye with placement of a silicon implant under local anesthesia. Post-operatively, the conformer was well-placed with mild discharge and congestion. Tissue samples were sent for histopathology and microbiology.
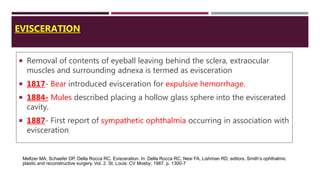
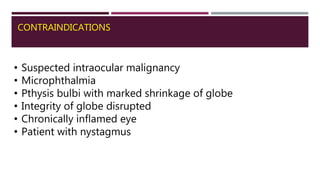
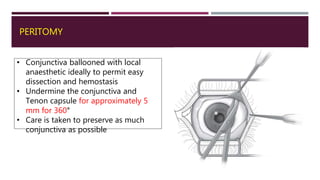
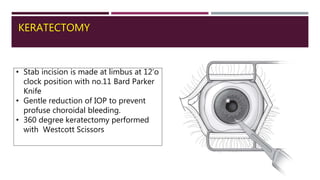
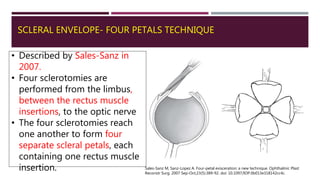
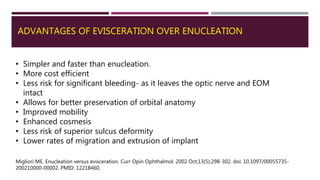
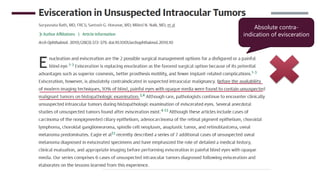
3. Evisceration involves removing the intraocular contents while leaving the external shell of the eye intact. It has advantages over enucleation such as being simpler
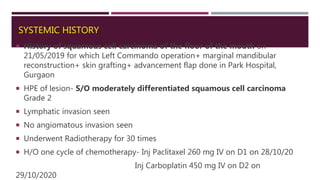





![COMPARISON OF POROUS AND NON POROUS IMPLANTS
Anterior migration
• Overall rate of implant migration
may be higher with porous
implants as compared to non
porous
Implant exposure
• Nonporous implants become
exposed– typically extrude from
the socket
• Porous orbital implants
become exposed--the
fibrovascular ingrowth helps
retain them within the orbit, often
preventing complete extrusion.
• Wladis et al. reported that rates
of exposure (and extrusion) are
generally comparable between
porous and nonporous
implants(1)
Infection Rate
• Nonporous implants (e.g.,
PMMA/silicone) have been shown
to have a low infection rate (0–
1%) [2]
Motility Rate
• Without a peg in place, there is
no proven motility advantage of
porous over nonporous implants.
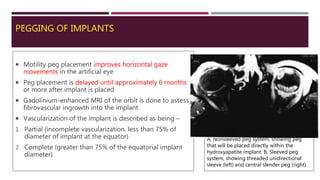
• Peg placement improves
horizontal gaze movements in
the artificial eye
1.Wladis EI, Aakalu VK, Sobel RK, et al. Orbital implants in enucleation surgery; a report by the American Academy of Ophthalmology. Ophthalmol 2017; 2017. pii: S0161–
6420(17)32438–7.
2. Hornblass A, Biesman BS, Eviator JA. Current techniques of enucleation: a survey of 5,439 intraorbital implants and a review of the literature. Ophthalmic Plast Reconstr Surg.
1995;11:77–88.](https://image.slidesharecdn.com/eviscerationandenucleation-210620063411/85/Evisceration-and-enucleation-65-320.jpg)