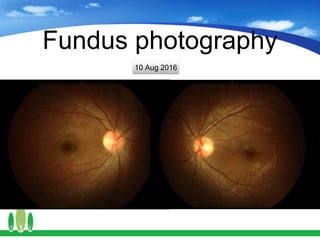
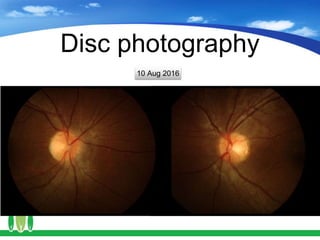
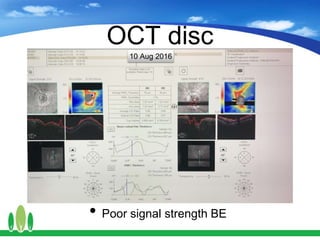
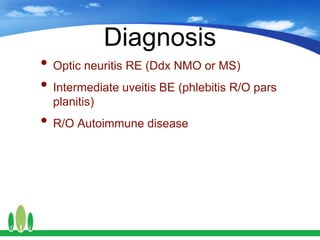
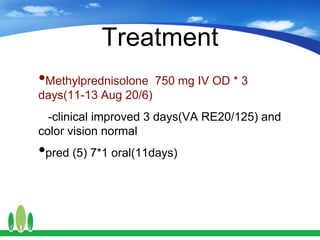
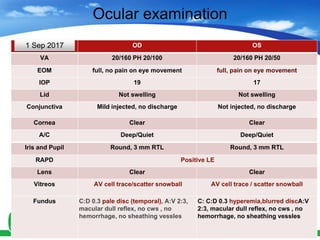
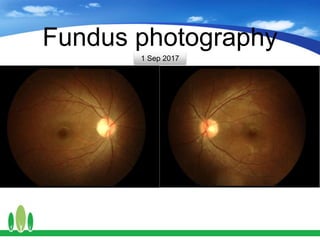
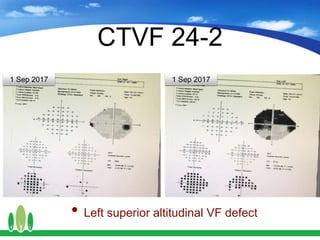
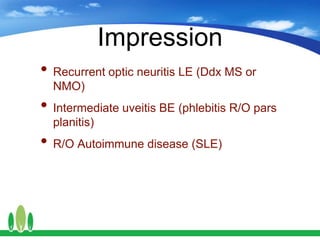
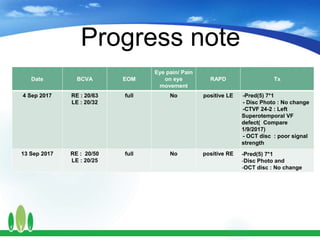
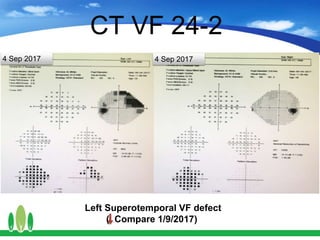
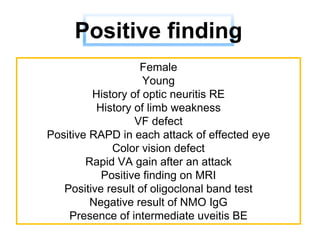
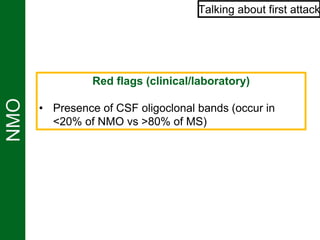
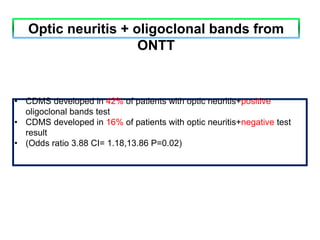
The document details a case of an 18-year-old female with recurrent optic neuritis, presenting with left eye pain and acute visual loss, alongside various diagnostic tests including MRI and laboratory results indicating possible autoimmune disease. Treatment involved methylprednisolone and prednisolone, with follow-ups showing improvement in visual acuity, but ongoing concerns regarding the potential diagnosis of multiple sclerosis (MS) versus neuromyelitis optica (NMO). The case emphasizes the complexity of diagnosing optic neuritis and its associations with broader neurological conditions.