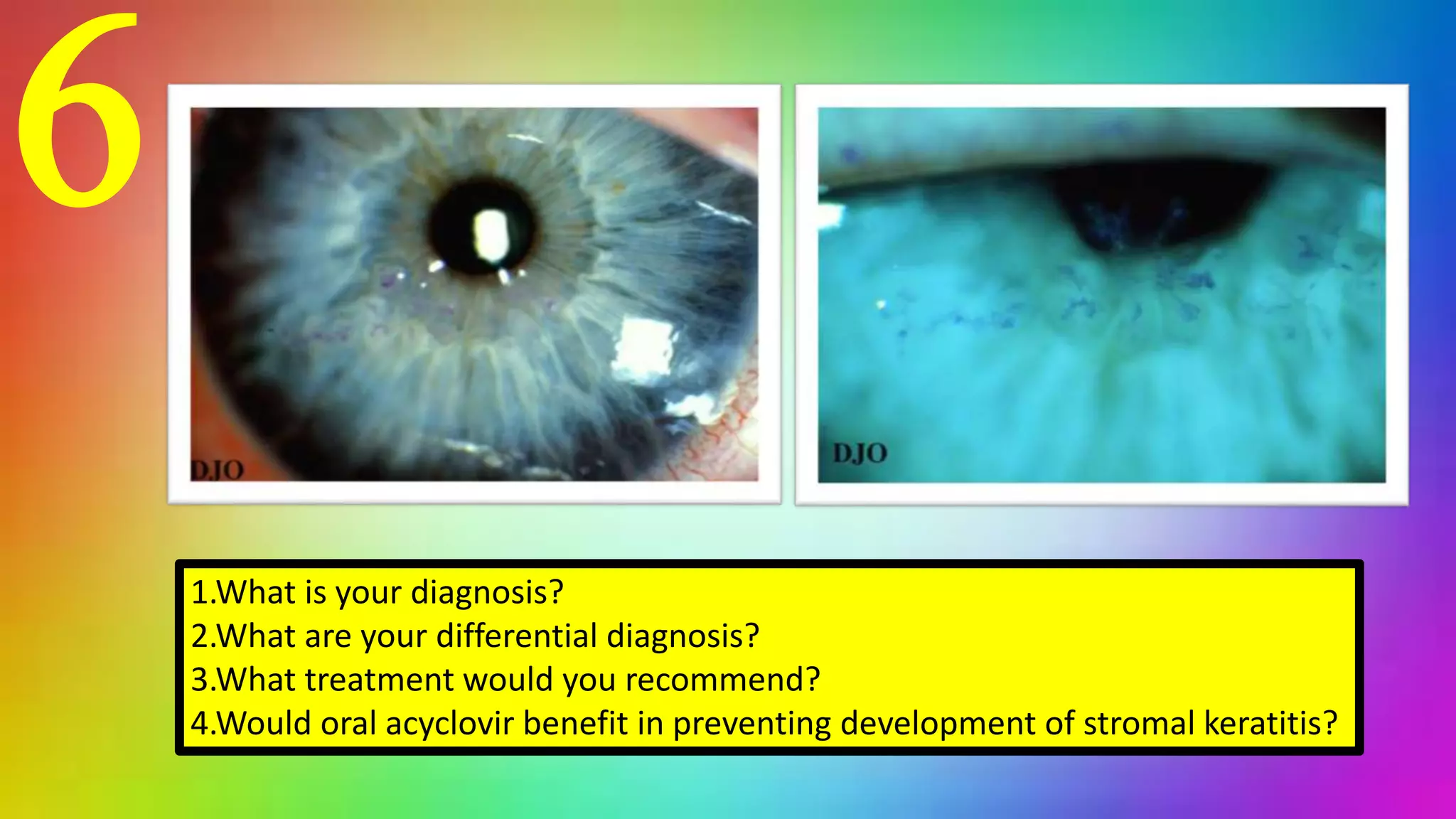
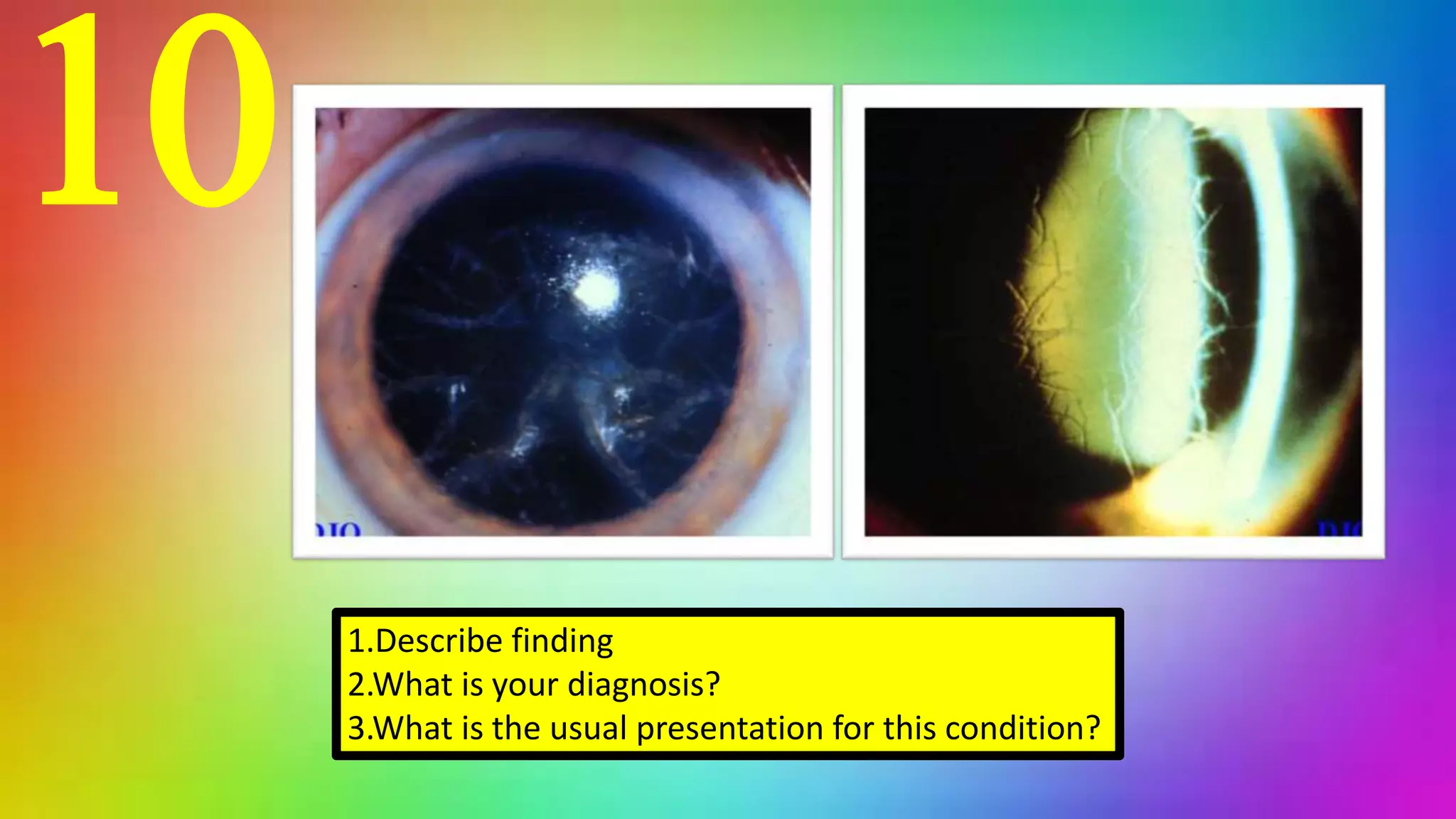
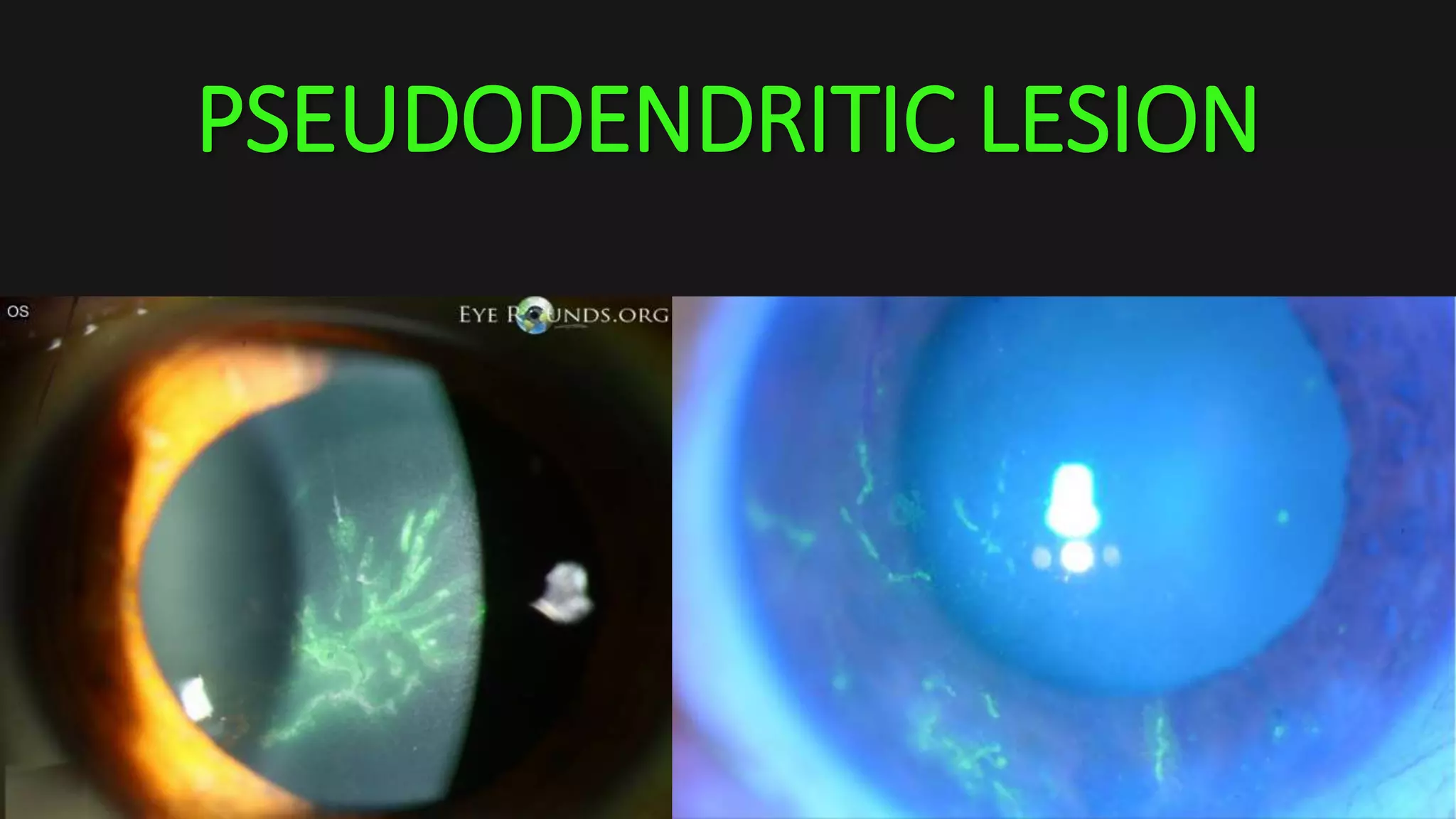
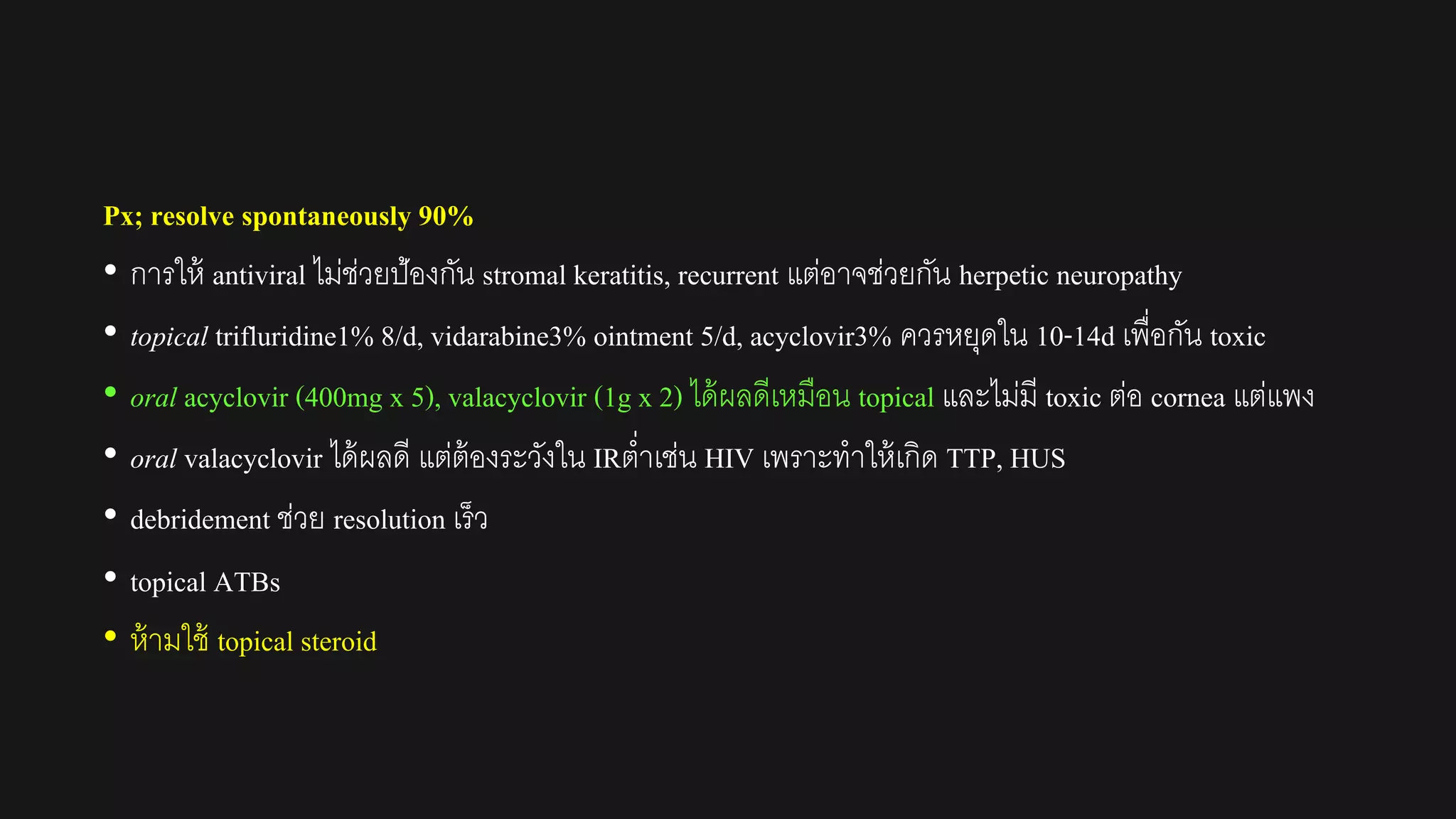
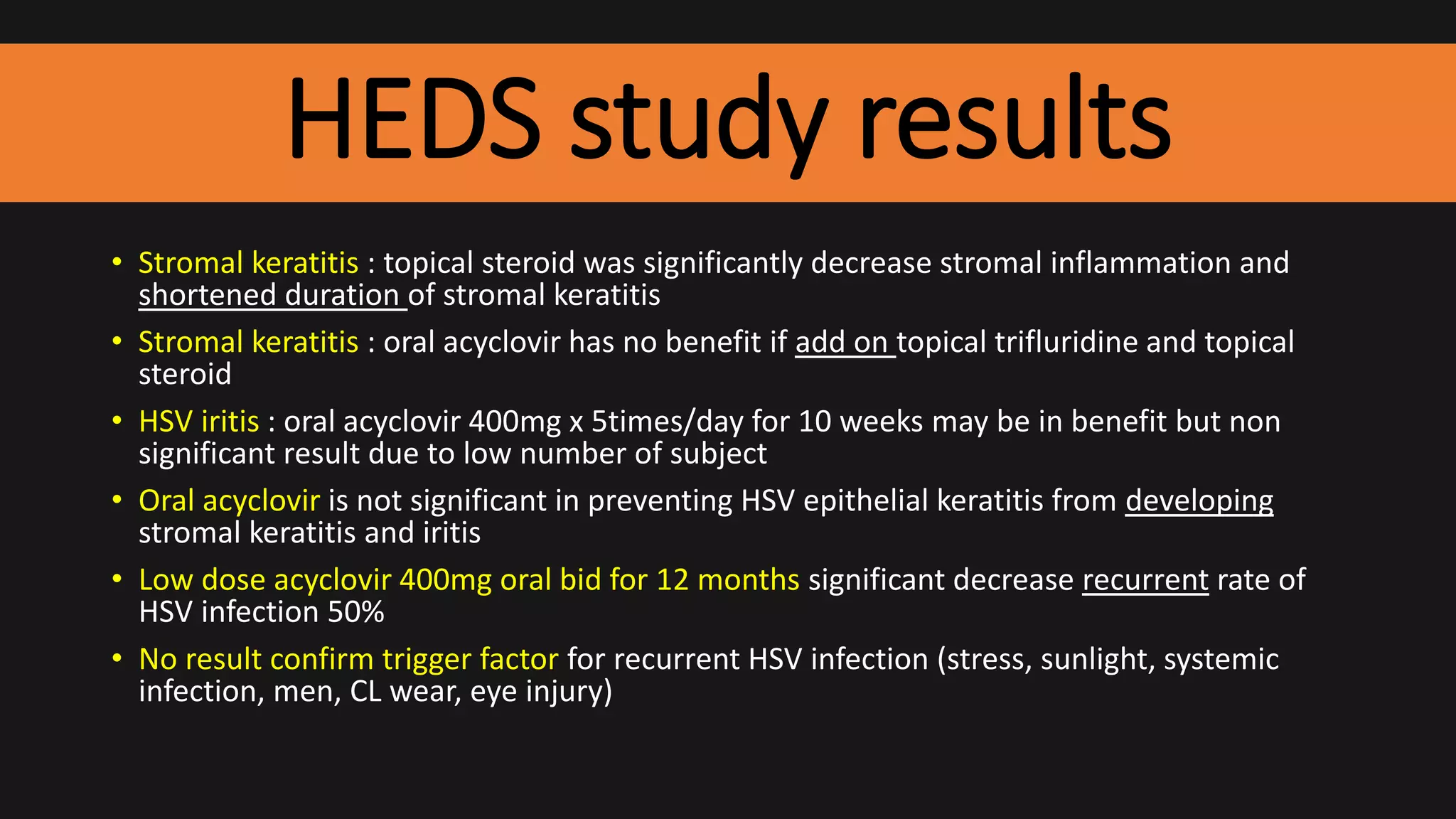
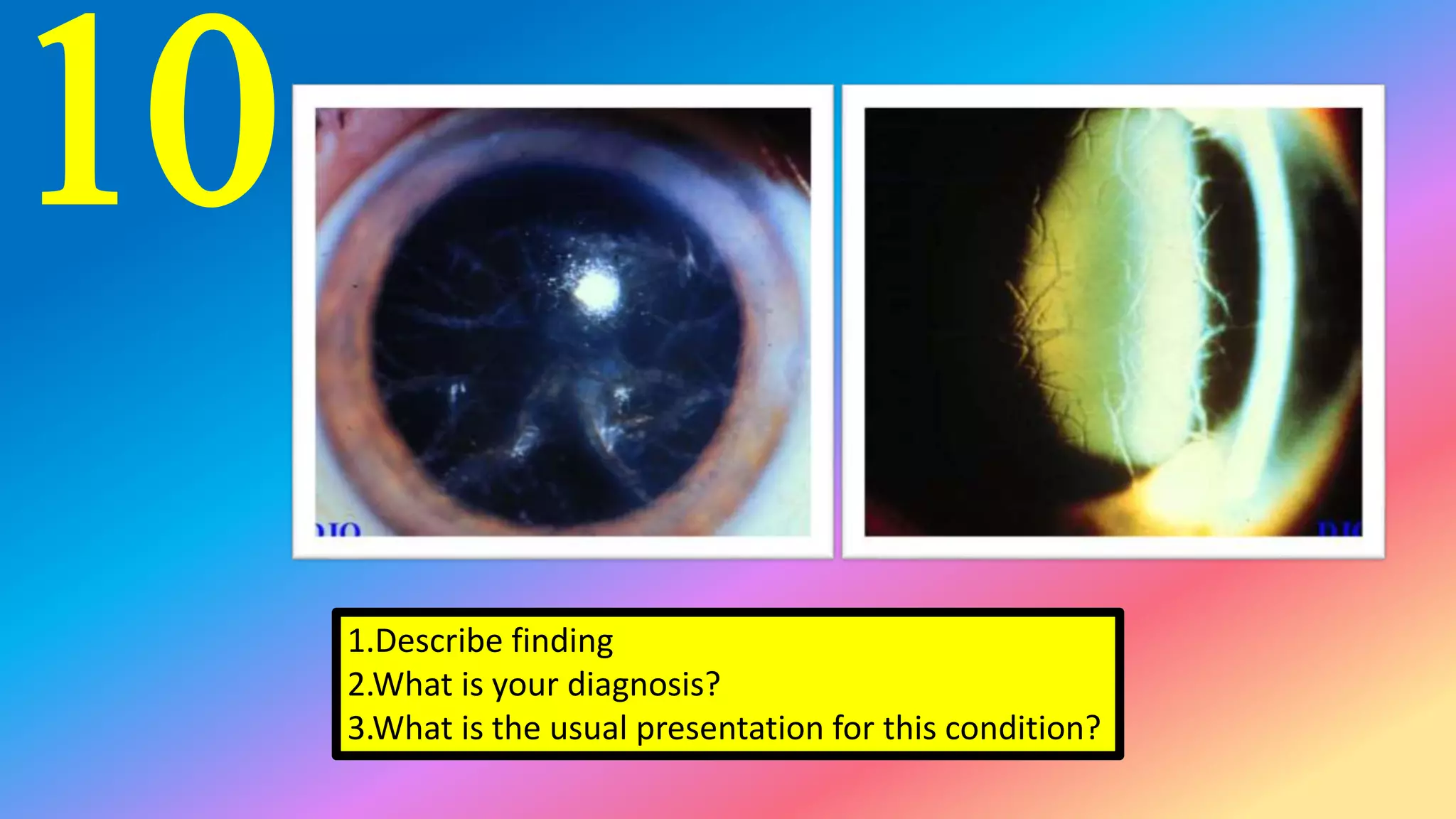
This patient presents with dendritic lesions and terminal bulbs on their cornea. The diagnosis is herpes simplex keratitis. Differential diagnoses include herpes zoster keratitis, healing recurrent erosion, soft contact lens wear. Treatment recommended is trifluorothymidine 1% eye drops 9 times per day or alternatively 3% vidarabine ointment 5 times per day. Oral acyclovir would not benefit in preventing development of stromal keratitis.