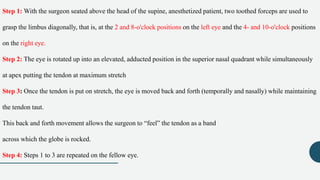
The forced duction test is used to evaluate restrictions of ocular muscle movement. It involves applying topical anesthesia and using forceps to gently rotate the eye in different gazes while feeling for resistance, which could indicate a muscle restriction. A normal test feels gradual resistance, while an absolute restriction prevents any rotation past a certain point. Proper technique and interpretation are important to avoid false positives or negatives. The test helps diagnose muscle palsies or contractures and distinguish between different restriction types.