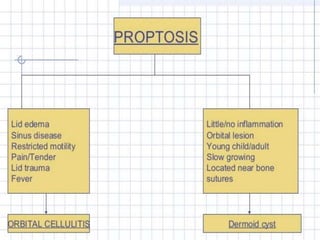
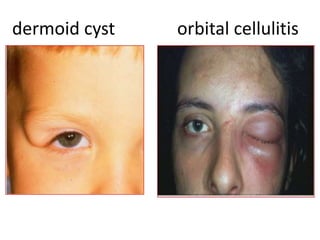
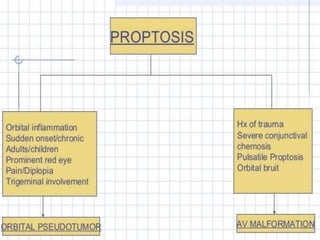
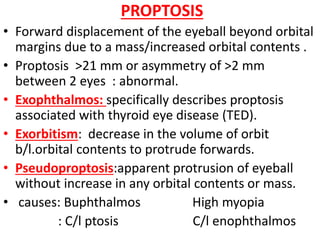
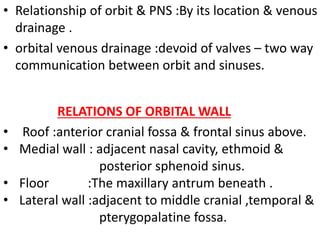
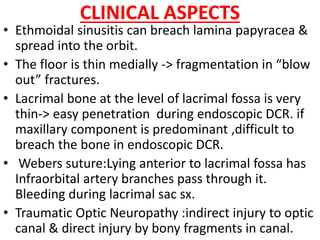
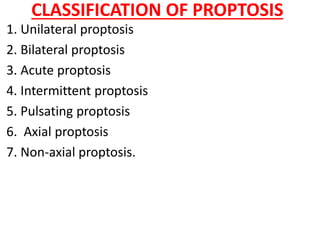
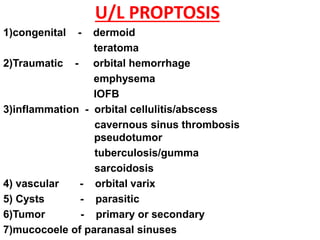
- Proptosis refers to forward displacement of the eyeball beyond the orbital rim, usually due to an increased mass or volume within the orbit. Common causes include tumors, inflammation, trauma, thyroid eye disease, and vascular lesions.
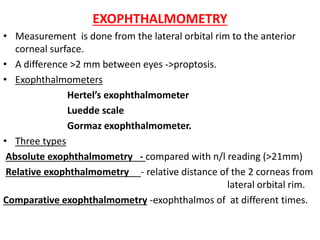
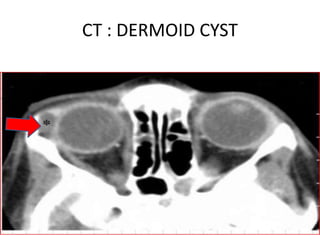
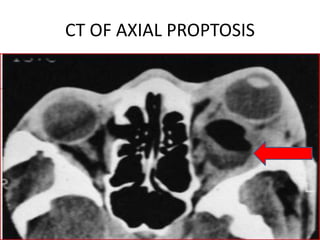
- Examination involves measuring exophthalmometry, inspecting for signs of mass effect, pulsation or displacement of the globe, and evaluating for neurologic deficits. Imaging with CT or MRI is important to characterize the lesion causing proptosis.


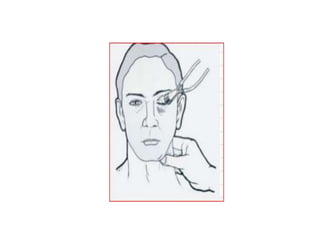
![OCULAR EXAMINATION
• Visual acuity, Refraction, visual fields, colour vision.
• Facial asymmetry,Head posture,Lid retraction/ptosis
• ocular alignment,Extraocular movements
• Examination of the anterior segment including pupil.
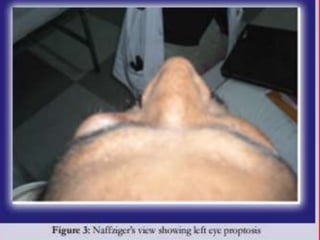
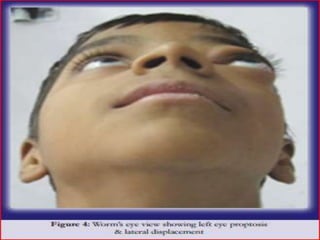
• INSPECTION:
• examiner looks from above standing behind patient/looks
up from below with the patient’s head tilted back
1]Type of proptosis (axial / non-axial),location of mass,
visible pulsation, skin changes.
2] Lagophthalmos,conjunctival congestion/discolouration.
3] Corneal exposure, change in size with valsalva.
4] examination of the globe and ocular adnexa
* Dilated episcleral vessels: arteriovenous shunt.](https://image.slidesharecdn.com/proptosis-170621161808/85/Proptosis-in-ophthalmology-24-320.jpg)
![*A “salmon patch” lesion beneath the upper eyelid:
orbital lymphoma, amyloidosis, sarcoidosis, leukemia,
lymphoid hyperplasia, rhabdomyosarcoma.
*Eversion of the upper eyelid ->waxy yellow
infiltrate with tortuous vessels : amyloid lesion.
*S-shaped deformity of upper eyelid : plexiform NF.
PALPATION :
1] Size, shape, surface, margins,consistency.
2] Signs of inflammation, tenderness, reducibility,motility.
3] Variation with valsalva, resistance to retropulsion,Thrill.
4] Corneal sensation, infraorbital / supraorbital anesthesia
5] Any swelling around the eyeball, regional lymph nodes
& orbital rim.
AUSCULTATION
abnormal vascular communications -> bruit
caroticocavernous fistula.](https://image.slidesharecdn.com/proptosis-170621161808/85/Proptosis-in-ophthalmology-25-320.jpg)