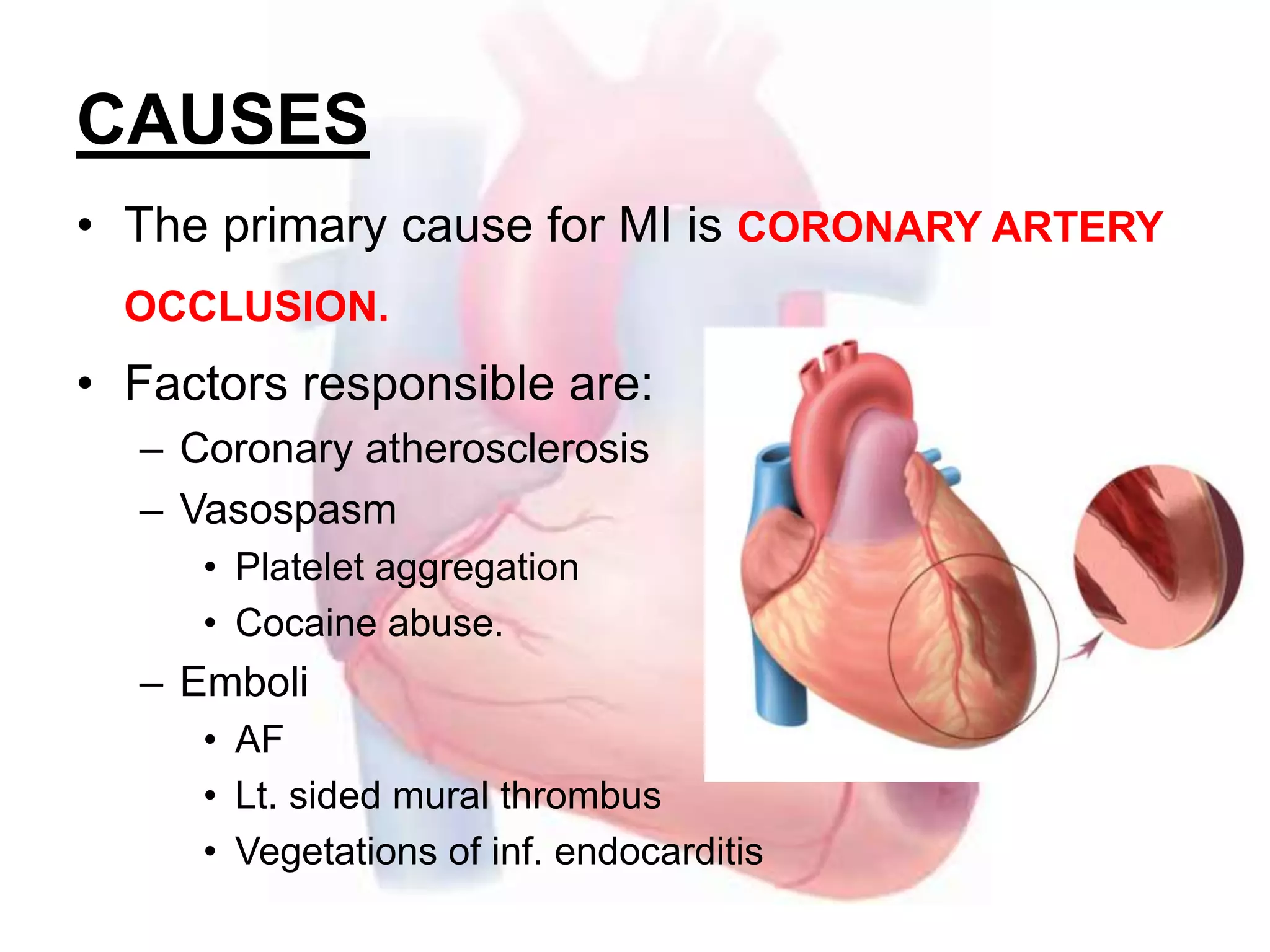
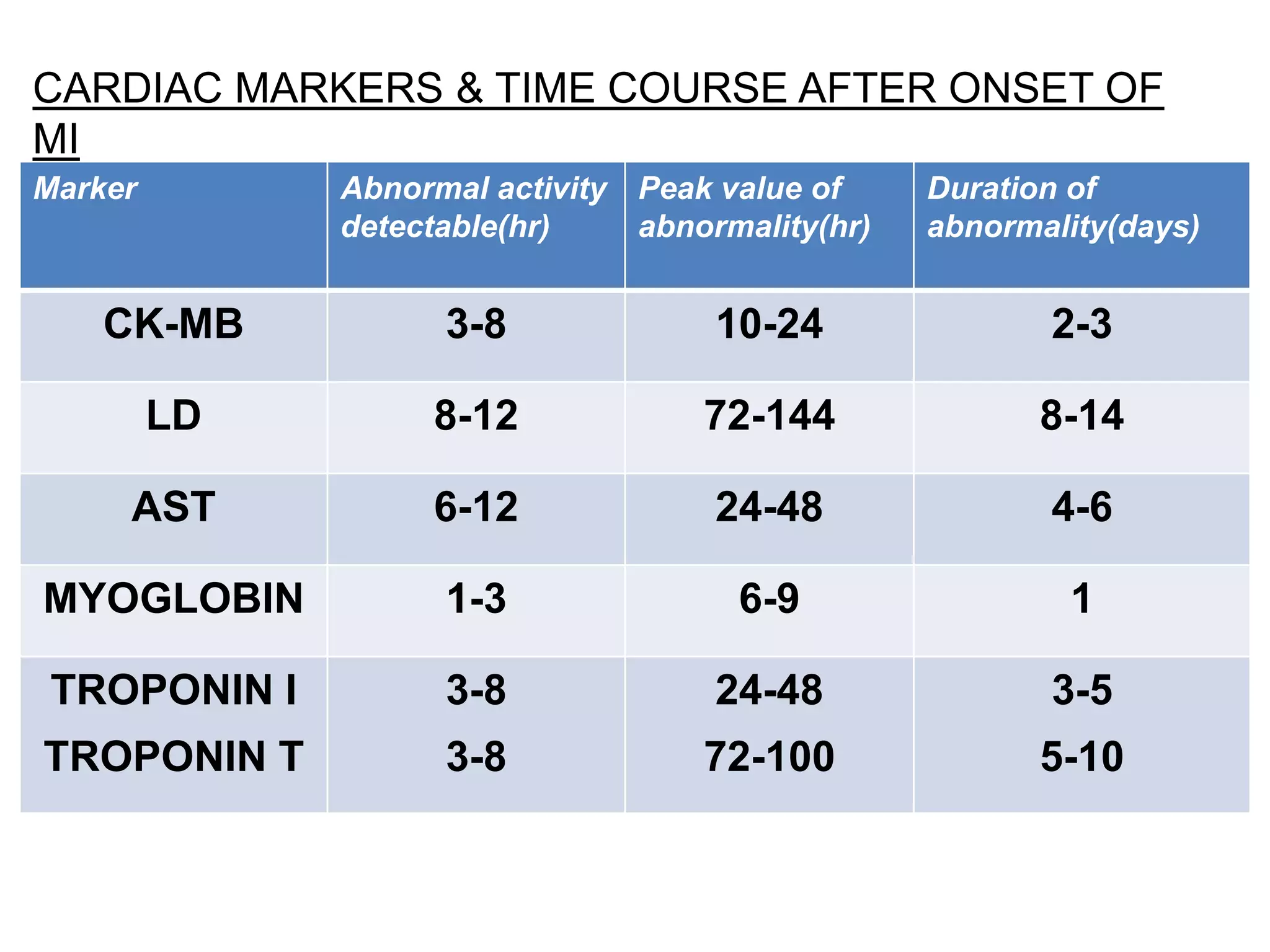
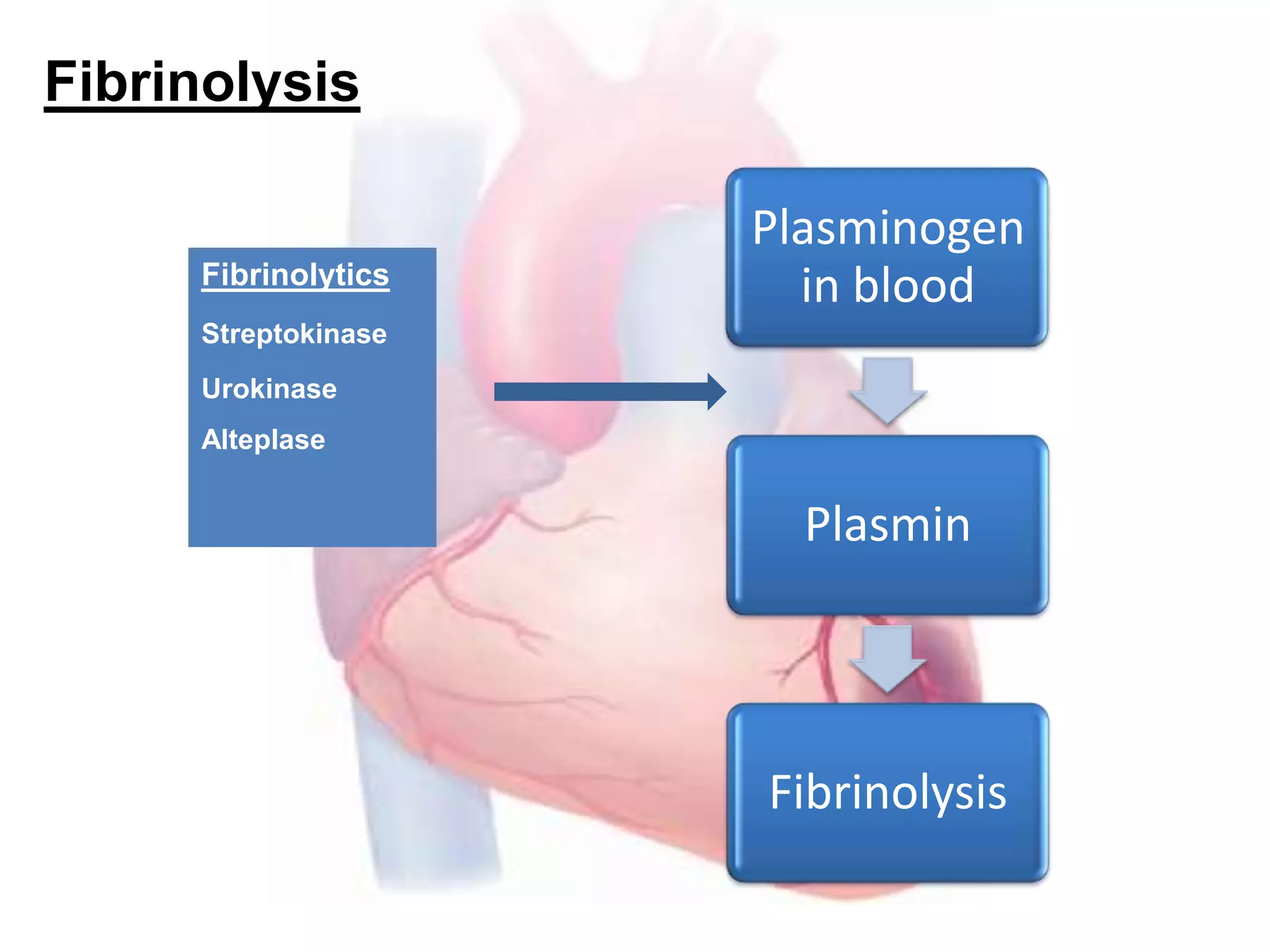
Myocardial infarction, also known as a heart attack, results from a critical imbalance between oxygen supply and demand in the heart muscle. The primary cause is coronary artery occlusion due to atherosclerosis, vasospasm, or embolism. Symptoms may include chest pain, dyspnea, sweating, and anxiety. Diagnosis is made based on elevated cardiac enzyme levels and ECG changes. Initial treatment focuses on pain relief, oxygen, fluids, and aspirin while long-term prevention includes medications like beta-blockers, ACE inhibitors, antiplatelets, and statins to reduce risk of future heart attacks and heart failure.