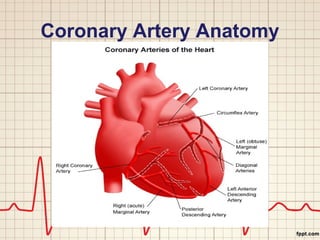
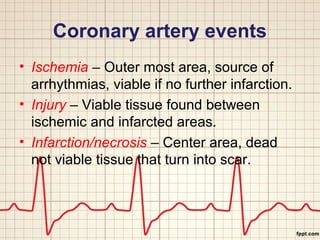
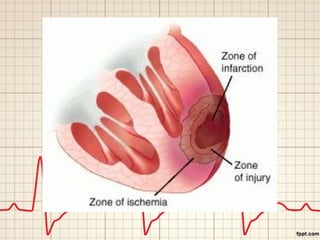
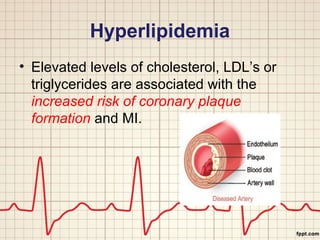
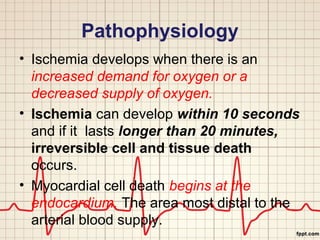
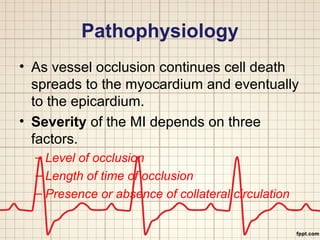
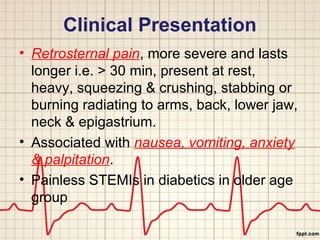
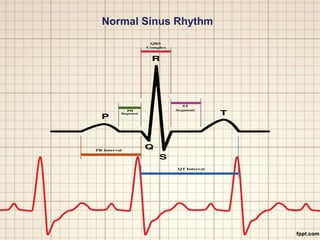
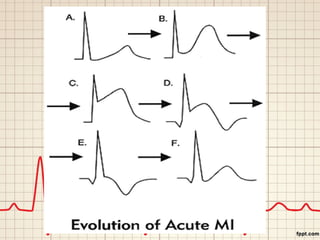
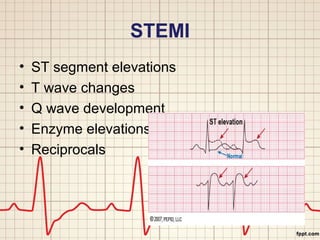
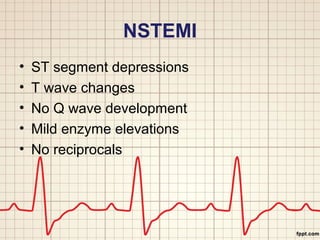
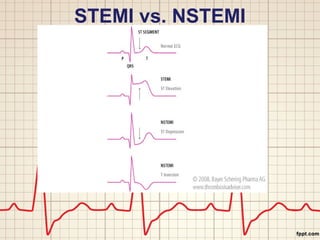
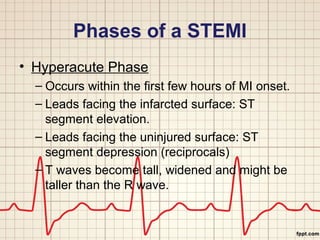
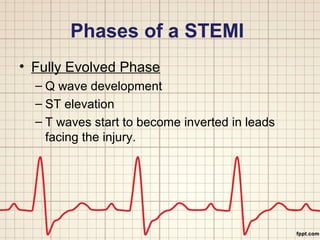
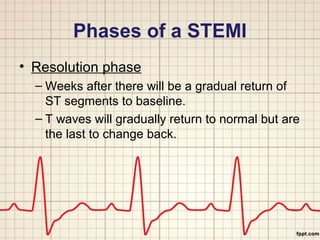
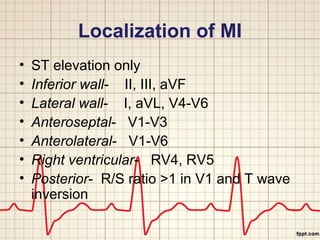
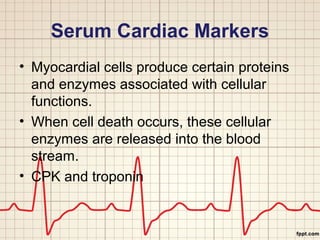
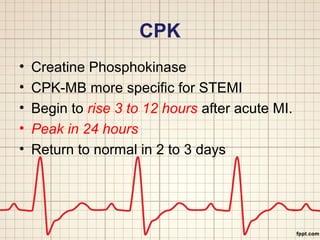
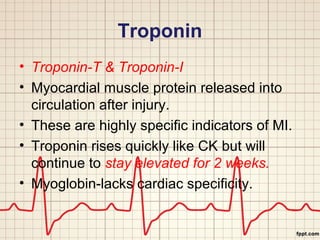
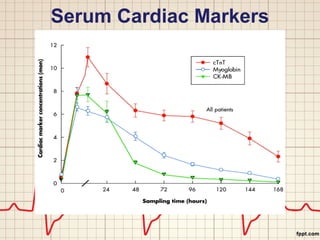
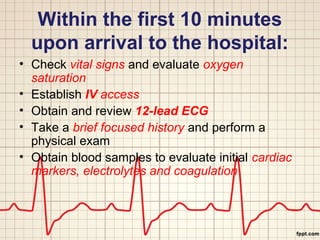
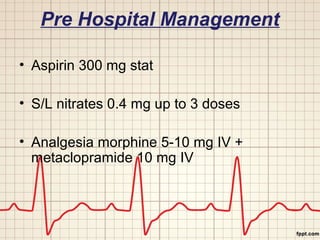
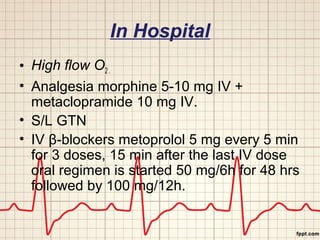
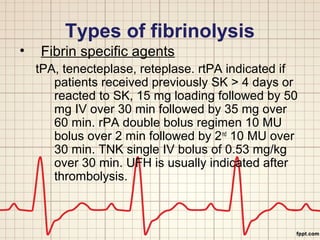
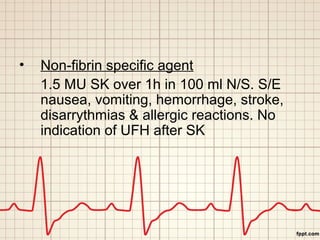
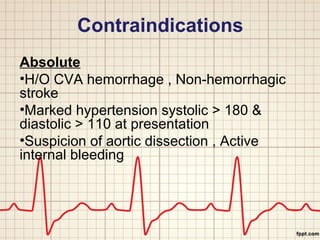
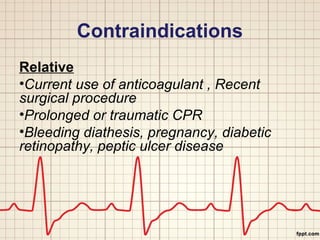
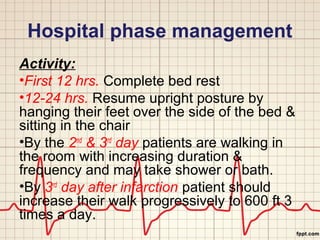
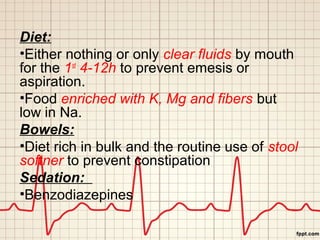
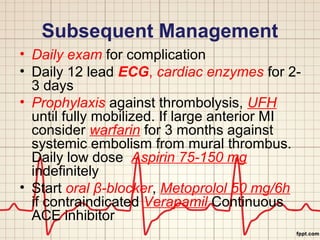
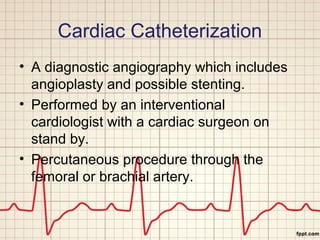
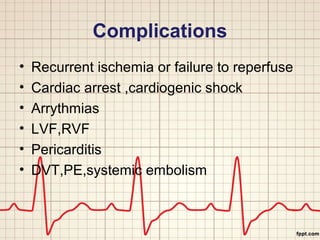
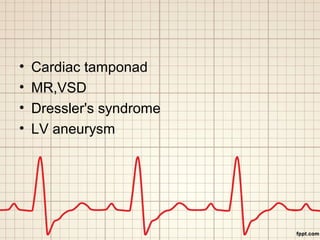
This document provides an overview of myocardial infarction (MI), also known as a heart attack. It defines MI as diminished blood supply and cell damage in the heart muscle. Risk factors include age, gender, family history, smoking, diabetes, hypertension, hyperlipidemia, obesity, and physical inactivity. Symptoms range from chest pain to breathlessness. Diagnosis involves ECGs, cardiac enzyme levels, and cardiac imaging. Treatment depends on whether the MI is STEMI or NSTEMI and may include medications, fibrinolytic therapy, angioplasty, and lifestyle changes to modify risk factors.