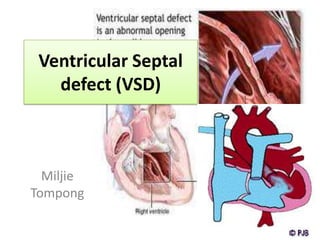
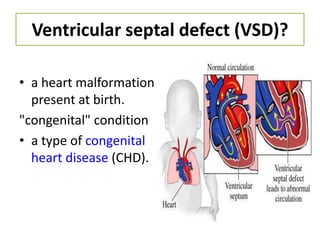
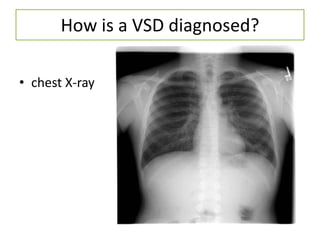
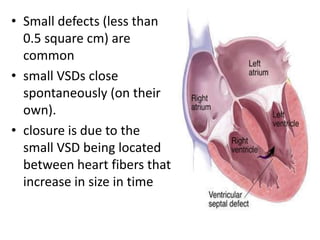
Ventricular septal defect (VSD) is a congenital heart defect where there is a hole in the wall separating the two lower chambers of the heart (ventricles). VSDs can range from small to large. Small VSDs often close on their own while large VSDs require medical or surgical treatment. VSDs are diagnosed using tests like echocardiograms, electrocardiograms, and chest x-rays. Treatment may involve medications to manage symptoms or surgery to repair the hole in the ventricle wall. Post-surgery, patients need monitoring and antibiotics to prevent infection.