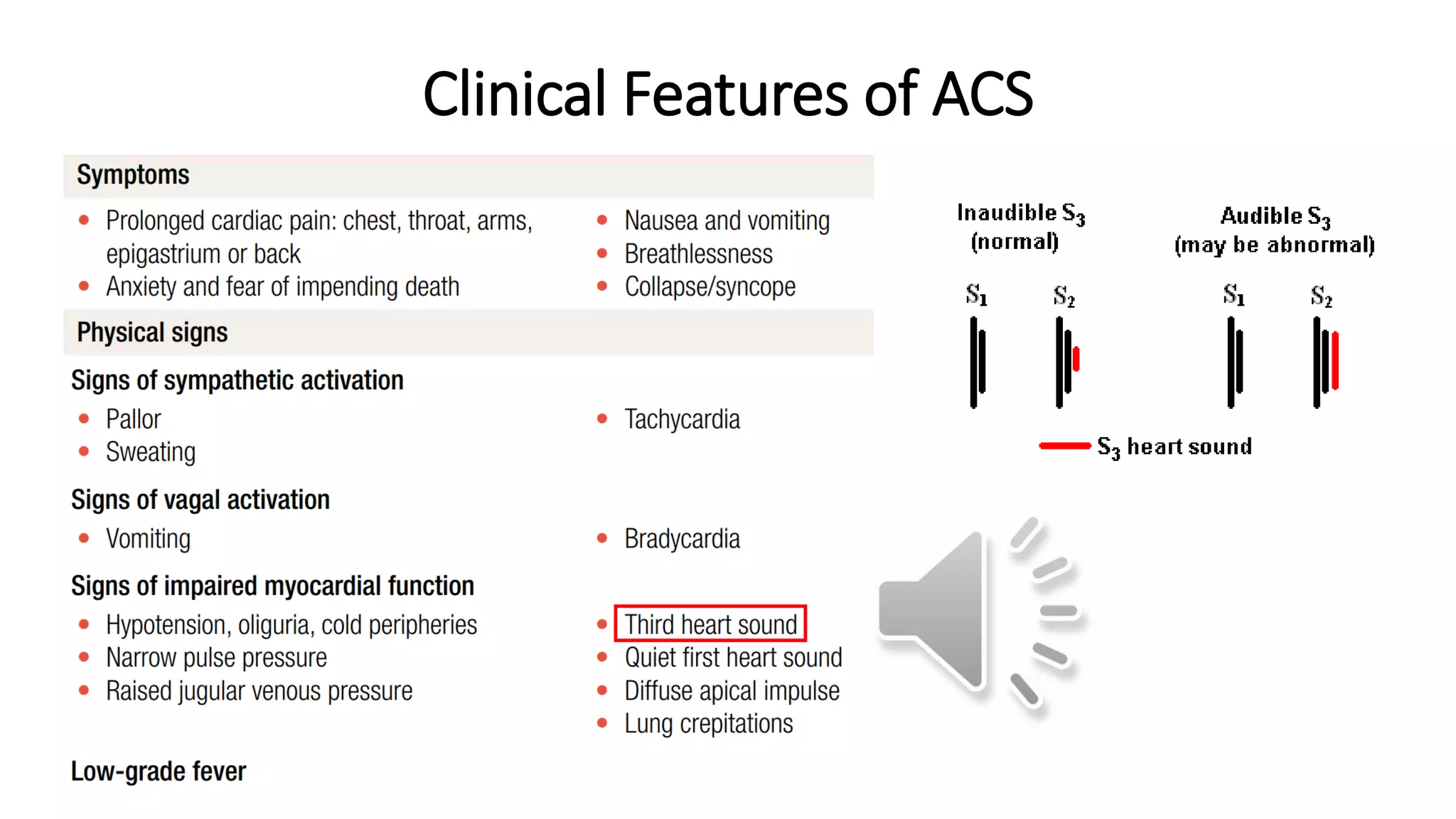
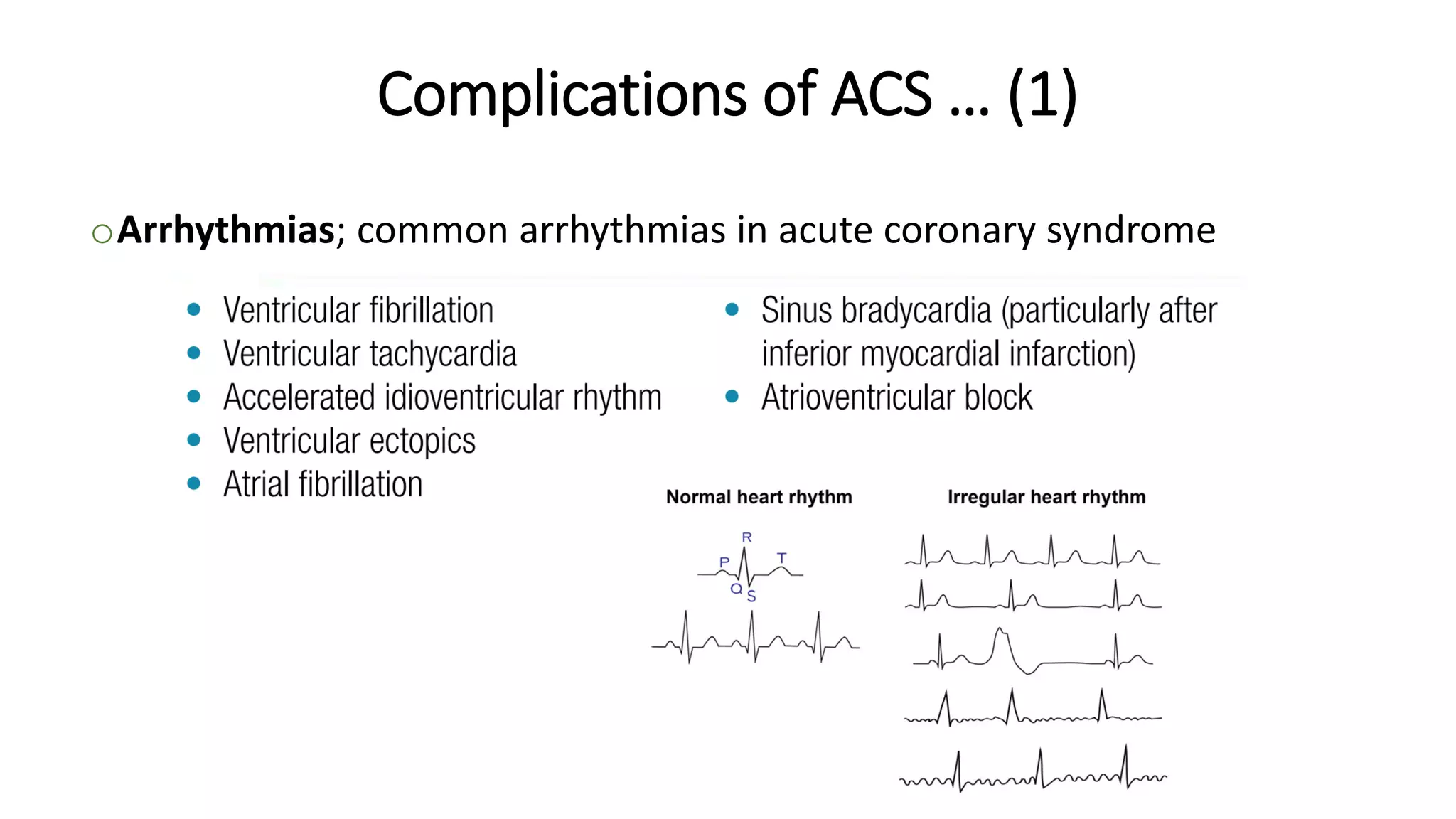
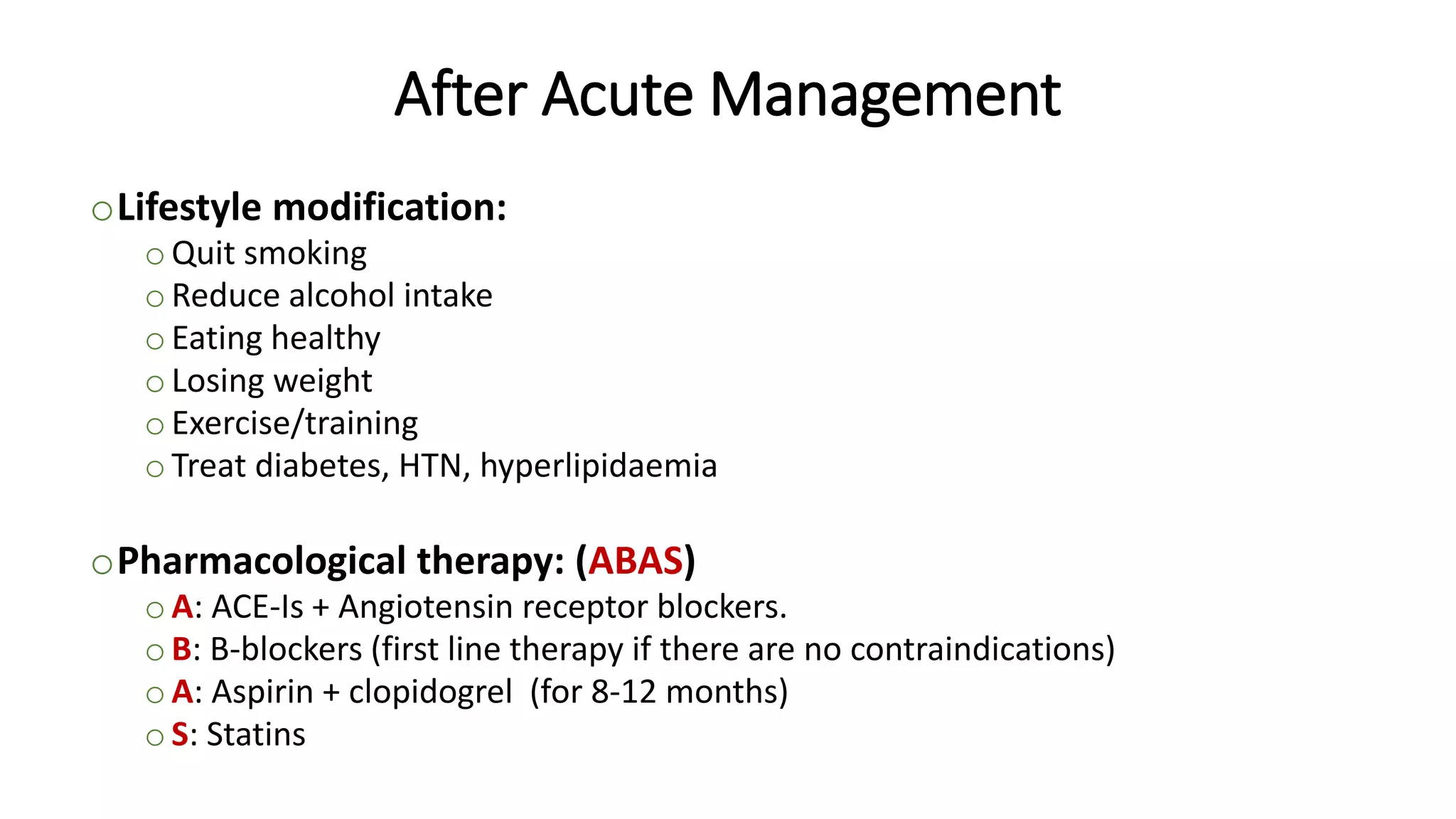
Acute coronary syndrome (ACS) encompasses unstable angina, NSTEMI, and STEMI, all resulting from acute obstruction of coronary arteries, leading to ischemic heart complications. Various clinical features and complications accompany ACS, including arrhythmias and post-infarct angina, with diagnosis primarily through ECG and cardiac biomarkers. Management includes hospitalization with continuous monitoring and treatment strategies such as medication and lifestyle modifications to prevent further events.