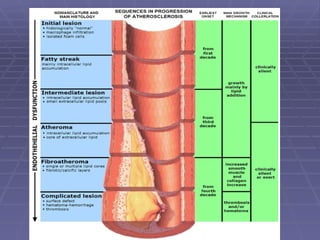
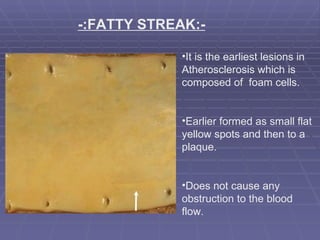
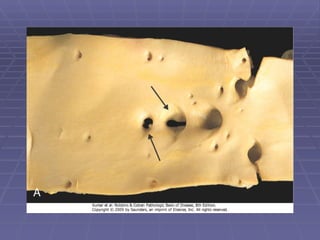
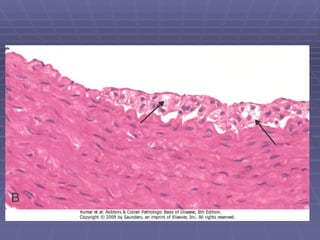
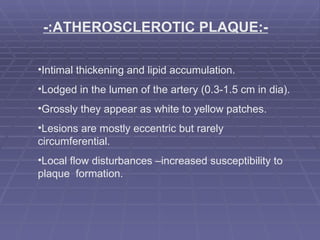
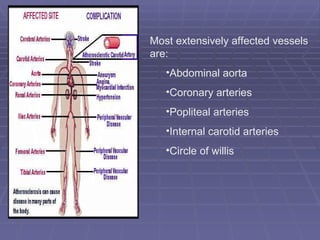
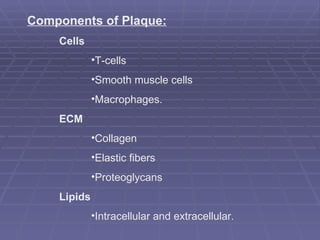
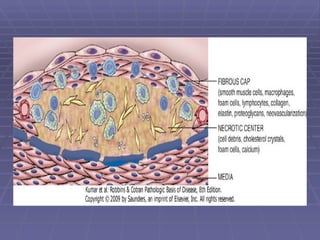
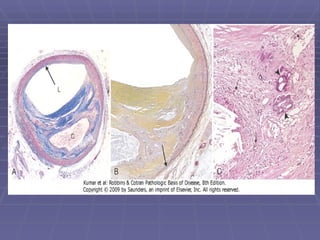
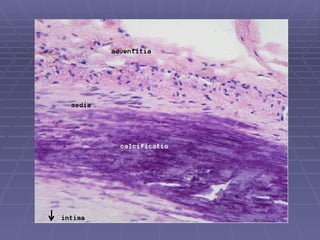
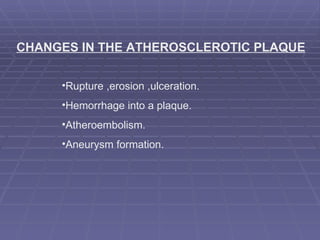
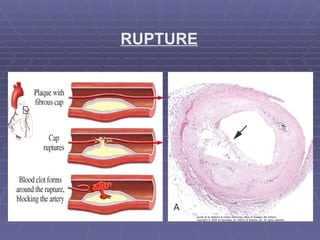
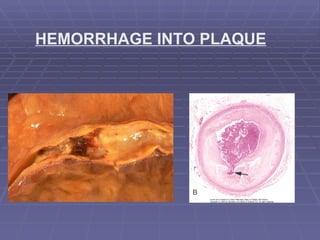
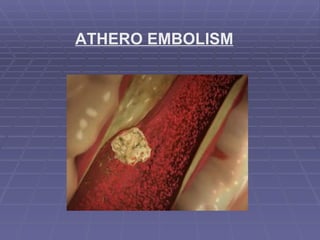
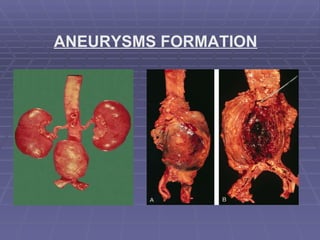
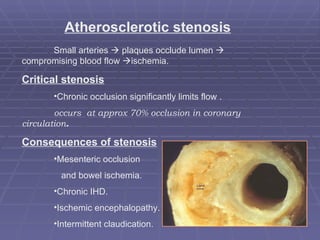
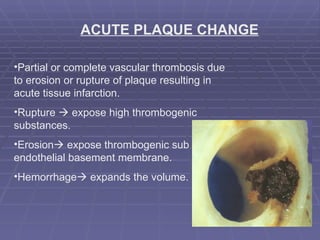
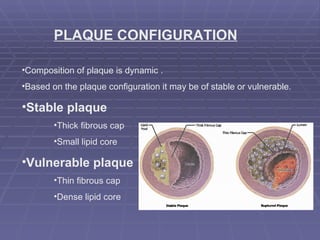
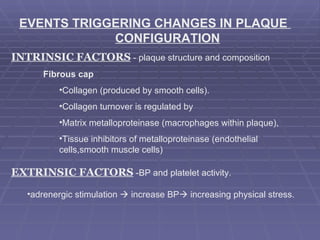
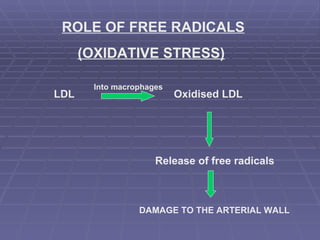
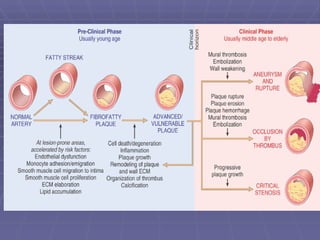
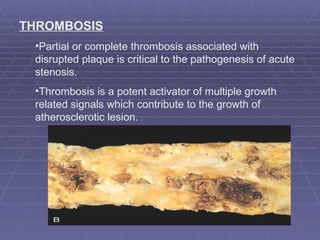
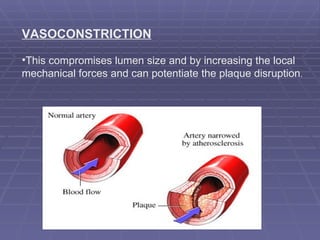
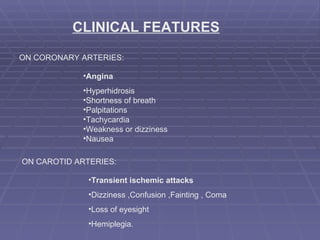
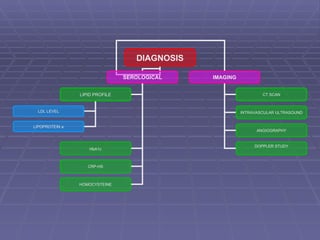
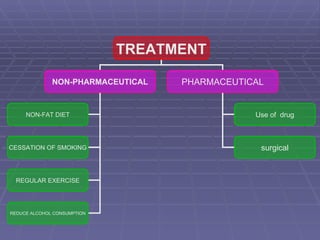
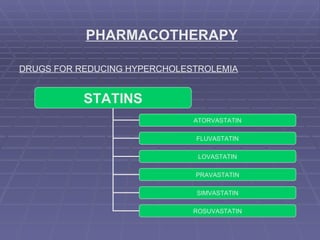
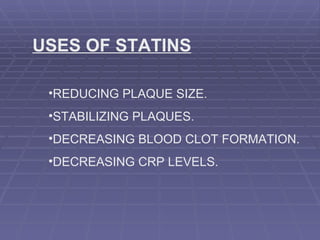
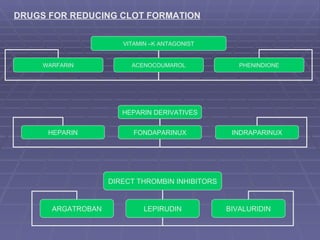
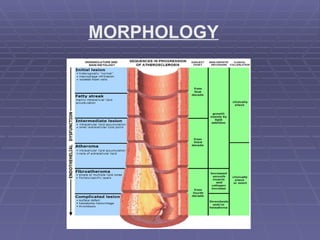
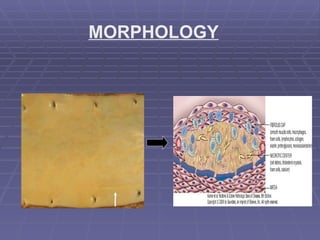
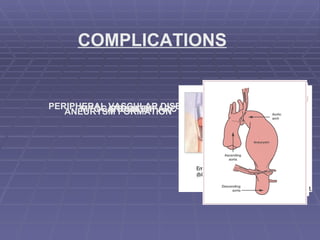
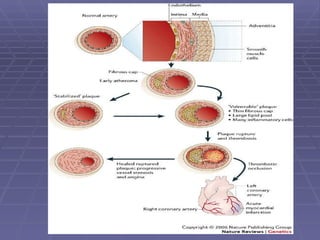
The document discusses the morphology and complications of atherosclerosis. It begins by describing the earliest lesion, the fatty streak, and later atherosclerotic plaques which form in arteries. Plaques are composed of cells, extracellular matrix, lipids, and can rupture or erode. This can lead to complications like myocardial infarction, stroke, and peripheral vascular disease. Diagnosis involves tests like CT scans and treatment includes lifestyle changes and medications like statins to reduce cholesterol and risk of clotting.