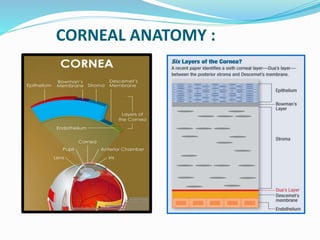
This document discusses techniques for measuring corneal thickness, known as pachymetry. It begins by introducing pachymetry and its importance in assessing corneal health and thickness. It then describes 12 techniques for measuring corneal thickness, including the gold standard of ultrasonic pachymetry. The document provides details on the principles, advantages, and disadvantages of each technique. It concludes by discussing the clinical utility of pachymetry in procedures like LASIK and for conditions like glaucoma and keratoconus.