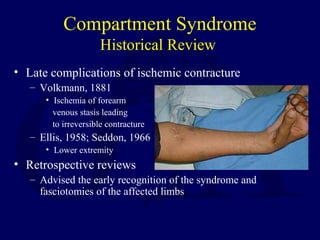
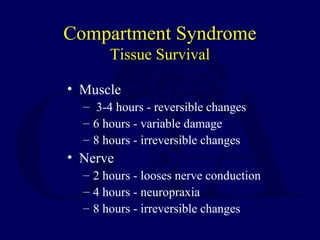
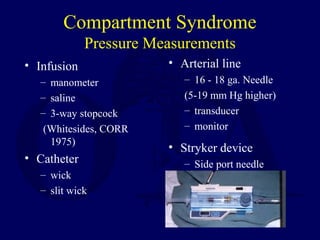
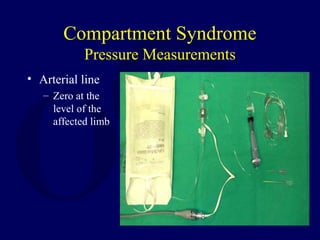
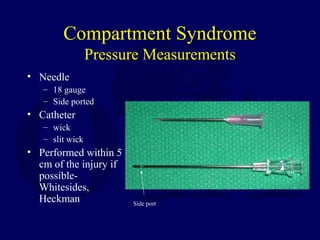
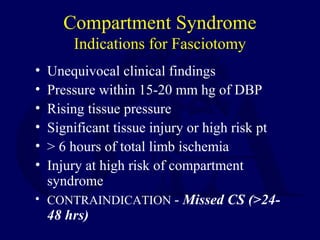
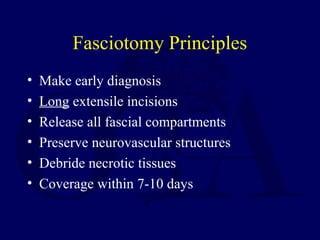
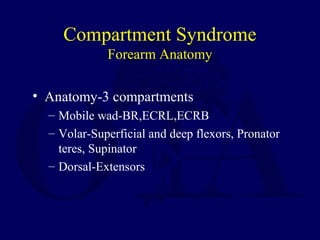
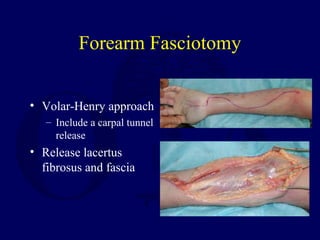
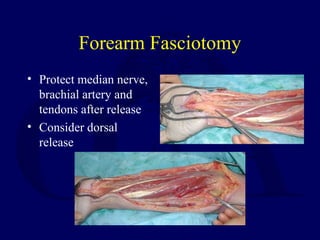
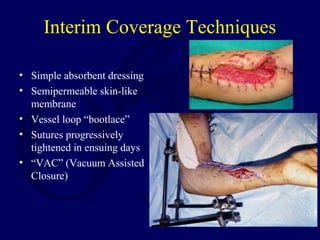
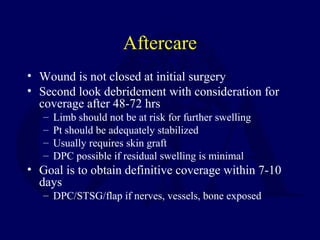
This document discusses compartment syndrome, beginning with definitions, pathogenesis, and a historical review. It then covers pathophysiology, including normal and elevated tissue pressures. Tissue survival times are provided for muscle and nerve damage. Etiologies and diagnostic criteria are outlined. Pressure measurement techniques and indications for fasciotomy surgery are described for various body areas like the forearm, leg, thigh, and foot. Post-operative care and potential medical-legal issues are also summarized.