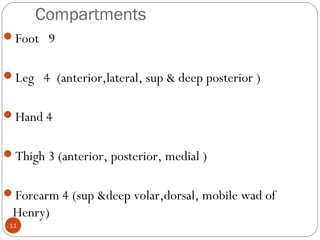
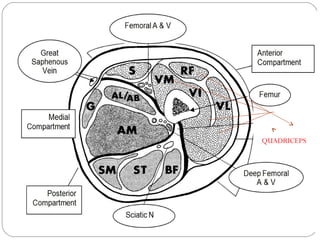
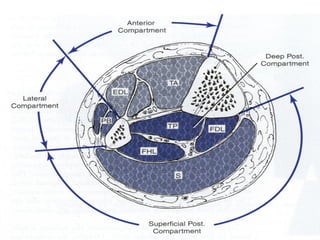
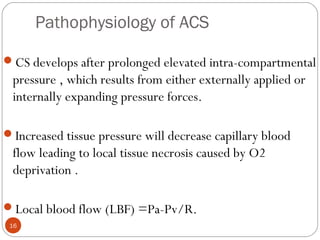
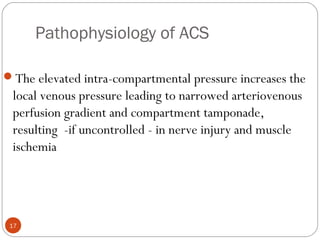
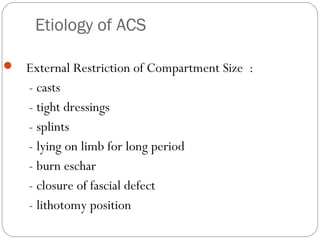
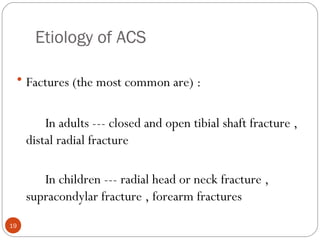
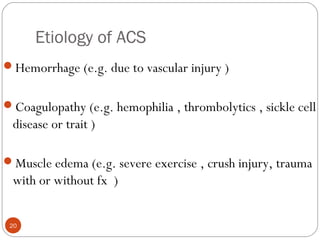
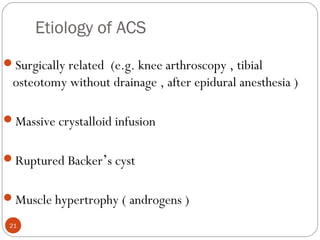
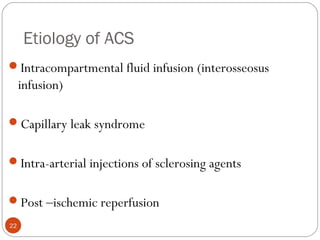
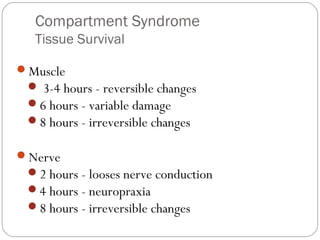
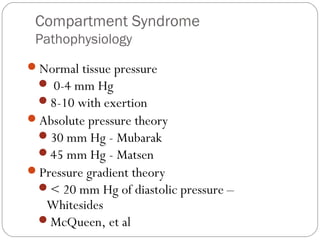
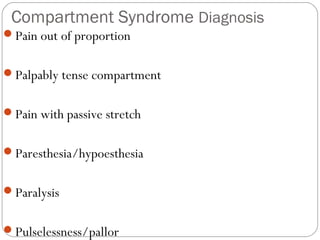
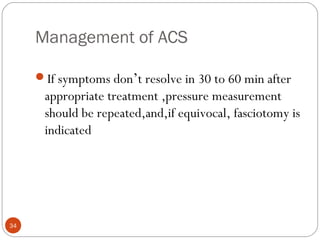
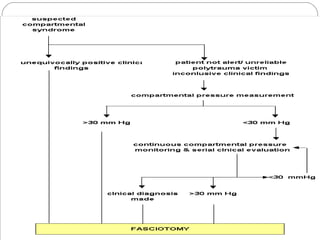
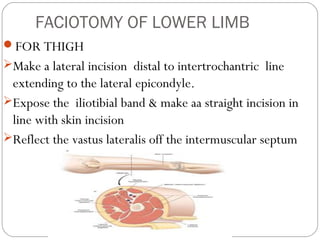
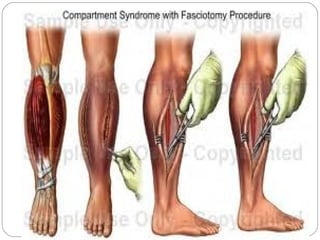
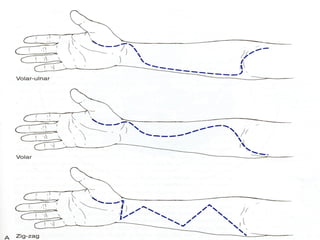
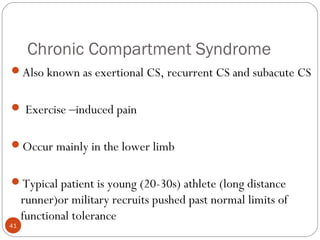
This document provides a history and overview of compartment syndrome. It discusses how compartment syndrome was first described in 1881 and the early studies identifying the condition and need for fasciotomy. It defines compartment syndrome as elevated tissue pressure within a closed space, describes the pathophysiology and risk factors. Diagnosis involves symptoms like pain out of proportion and tense compartments. Treatment is fasciotomy to release pressure if symptoms don't improve after conservative measures. Complications include contractures if not treated promptly.