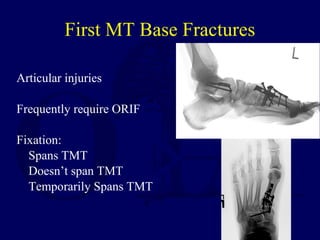
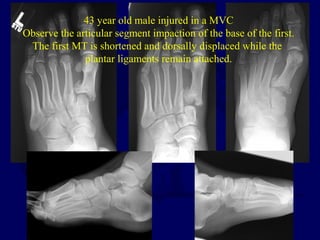
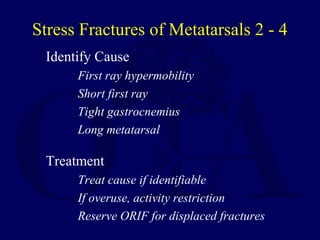
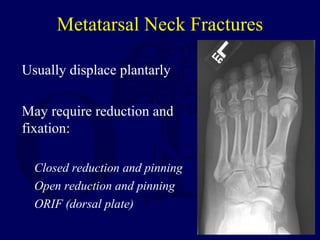
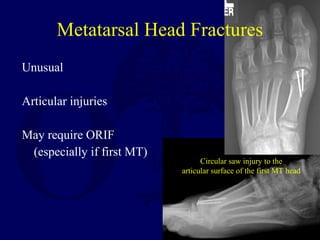
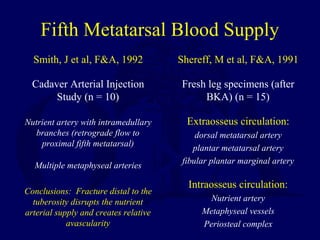
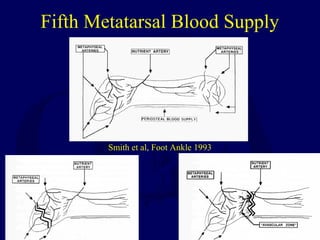
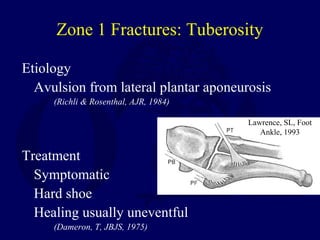
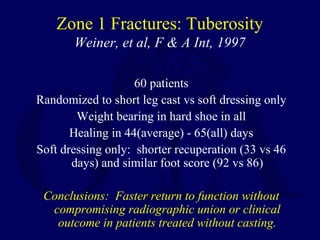
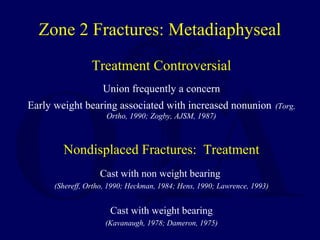
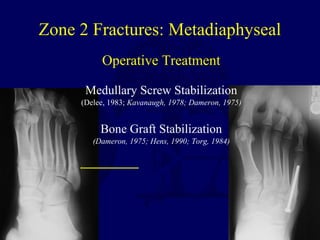
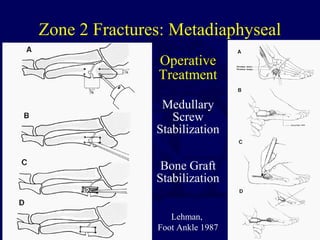
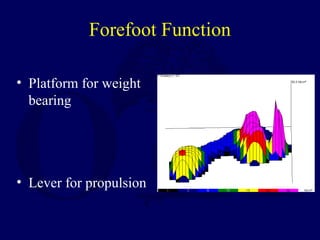
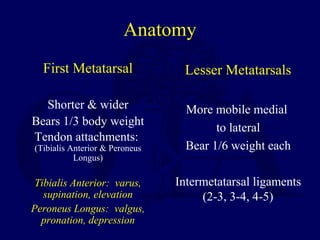
This document summarizes forefoot fractures, including anatomy, biomechanics, classification, and treatment principles. It describes fractures of the metatarsals, sesamoids, and phalanges. Treatment often involves closed or open reduction with pinning or plating to restore alignment and allow weight bearing. More comminuted fractures sometimes require bone grafting. Proximal fifth metatarsal fractures are classified into zones with implications for healing and management approaches.





![Biomechanics
Metatarsal heads in
contact with floor 60-
80% of stance phase
Toes in contact with
floor 75% of stance
phase
Cavanagh, PR, F&A, 1987
Hughes, J, JBJS[Br], 1990](https://image.slidesharecdn.com/l17-forefootfxs-161225233615/85/L17-forefoot-fxs-8-320.jpg)