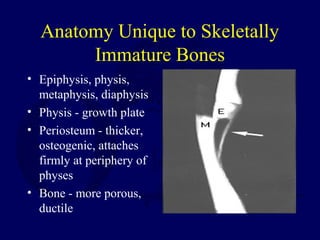
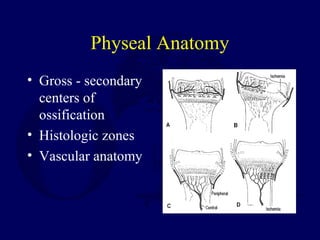
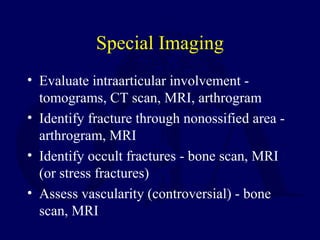
This document outlines the basic principles in assessing and treating fractures in skeletally immature patients. It discusses the unique anatomy of growing bones including growth plates, differences in examination and treatment approaches compared to adults, and complications that can occur such as growth arrest. The majority of pediatric fractures can be treated non-operatively with closed reduction and casting. Exceptions include displaced intra-articular fractures and physeal injuries which may require open reduction and internal fixation to achieve anatomic alignment. Overall, children generally heal faster than adults from fractures but treatment must account for the risk of disturbing growth.