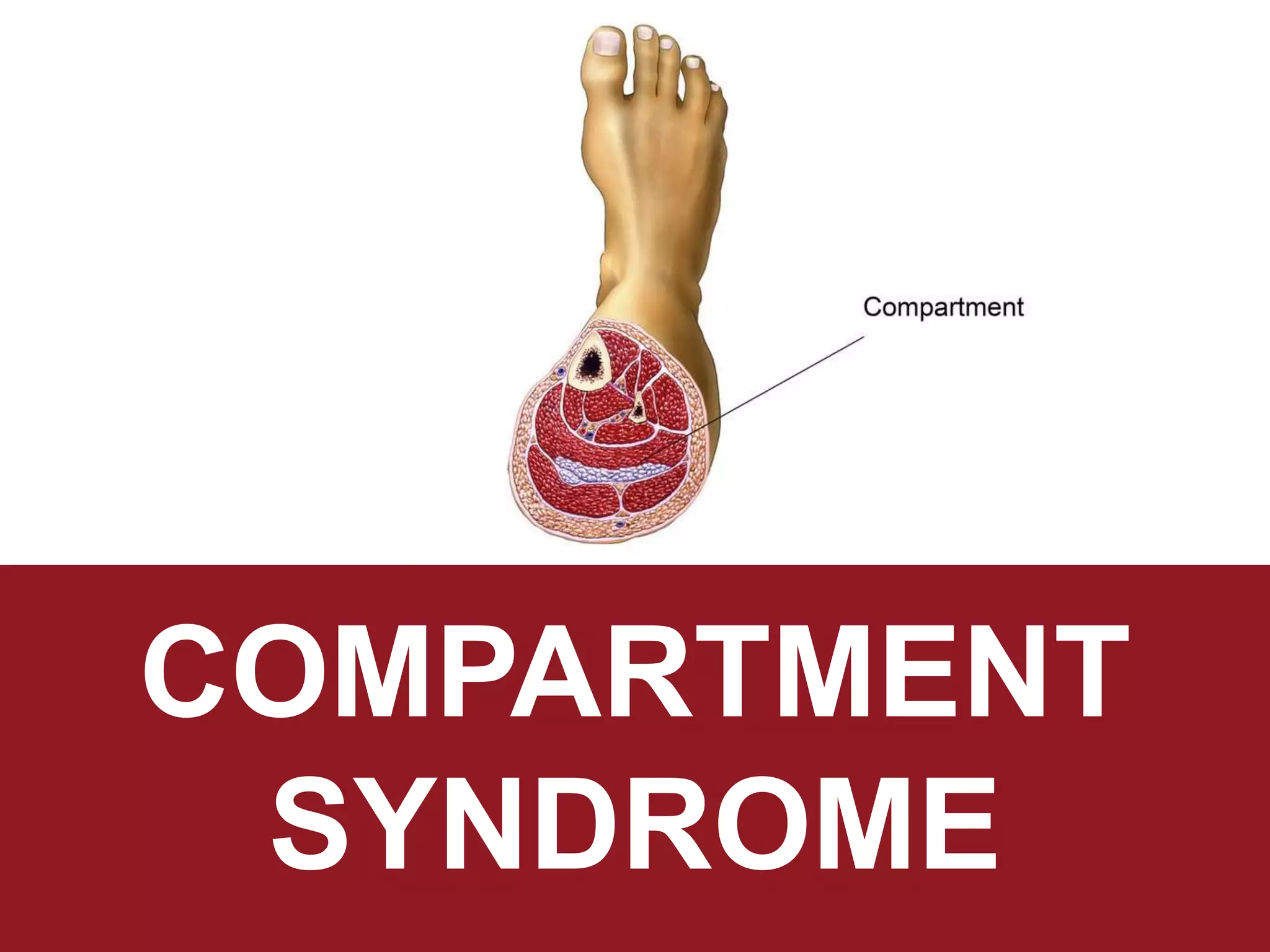
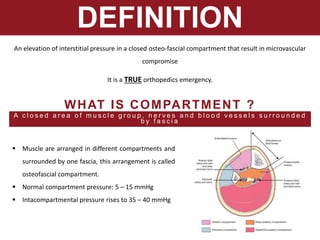
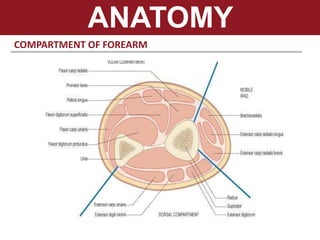
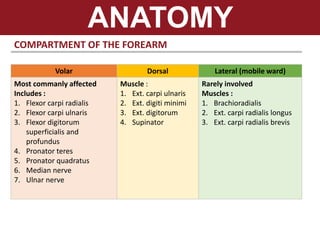
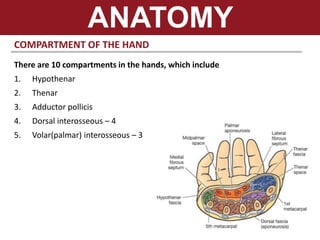
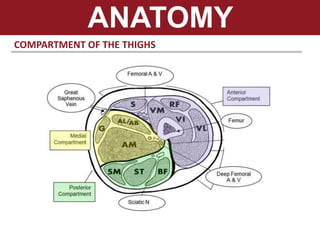
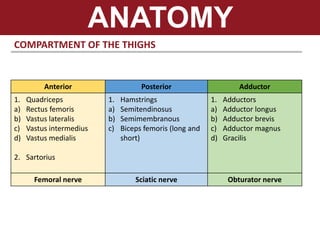
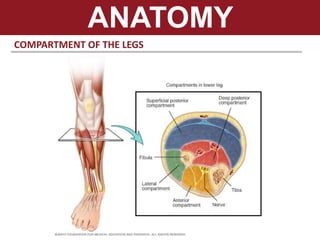
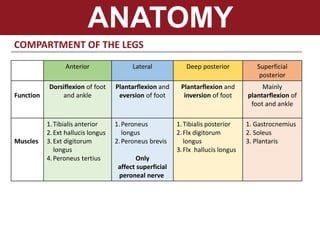
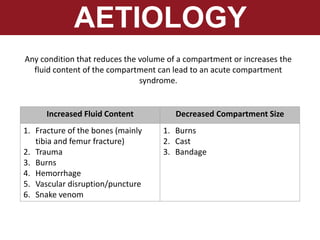
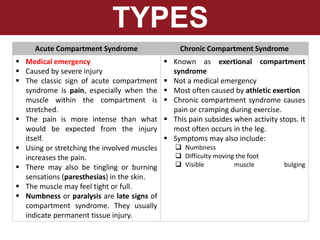
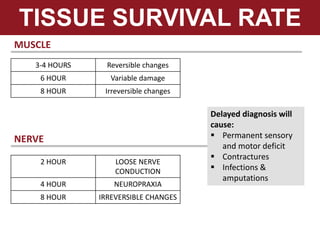
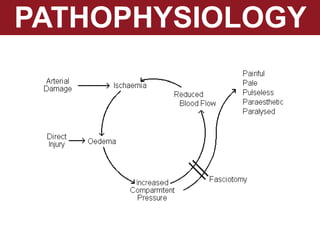
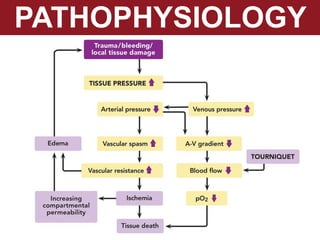
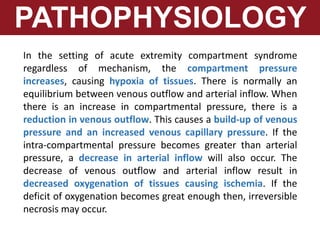
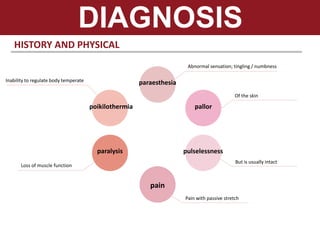
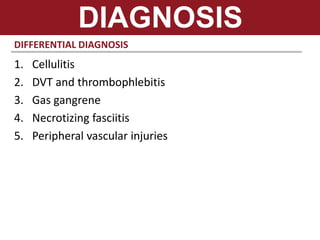
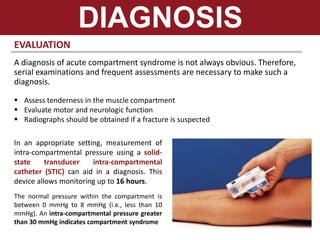
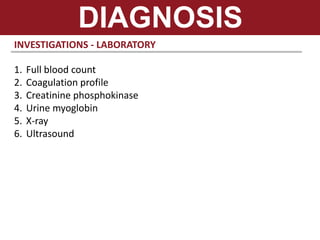
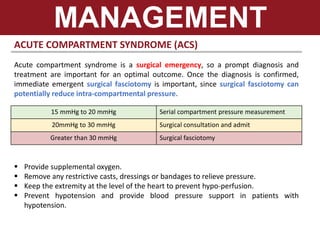
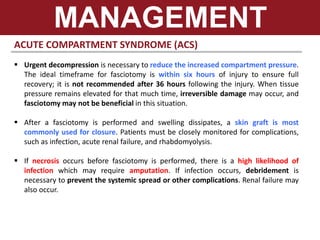
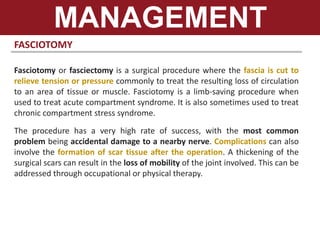
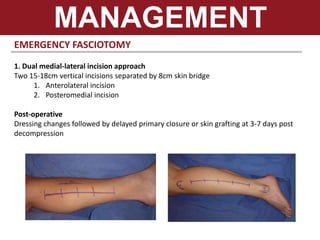
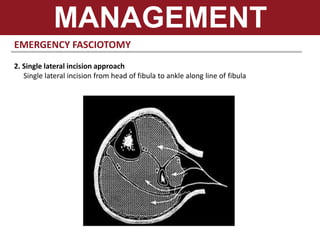
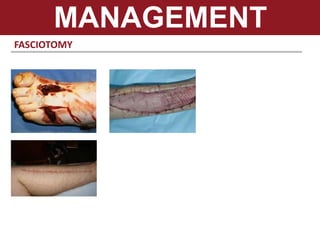
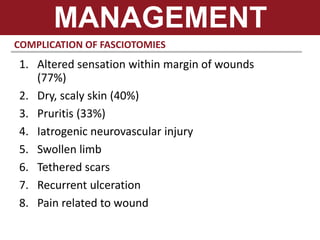
The document discusses compartment syndrome, a critical orthopedic emergency characterized by increased pressure within muscle compartments, leading to tissue ischemia. It outlines the anatomy of various compartments in the forearm, hand, thighs, and legs, common causes, symptoms of acute vs. chronic compartment syndrome, and the importance of timely diagnosis and surgical intervention. Management strategies include fasciotomy, addressing underlying causes, and careful postoperative monitoring to prevent complications.