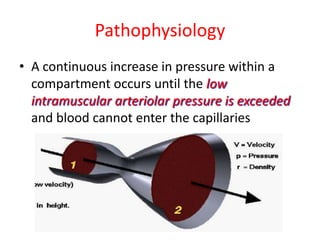
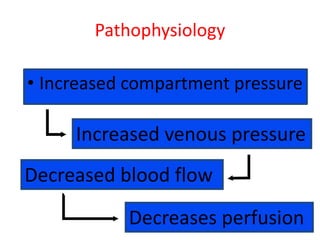
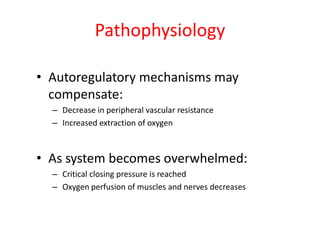
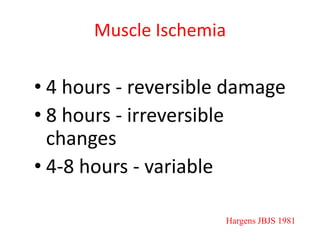
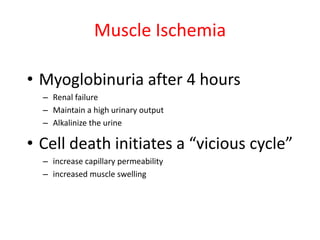
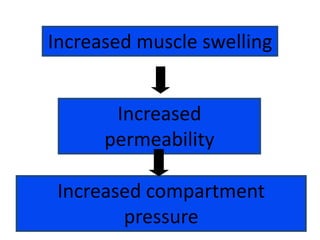
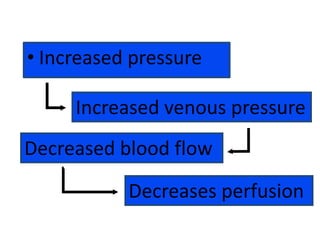
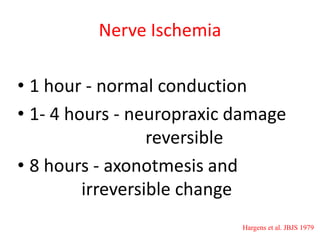
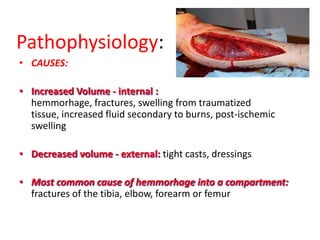
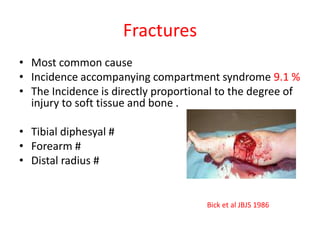
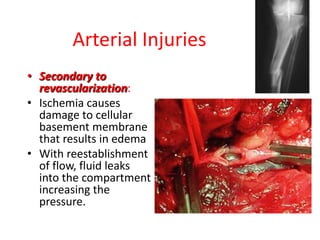
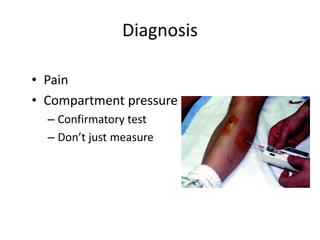
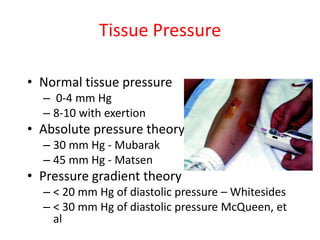
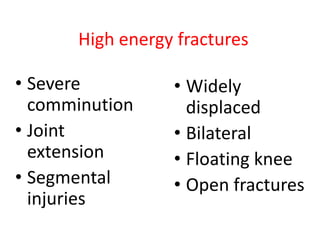
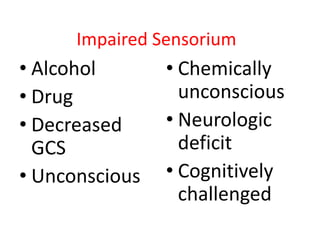
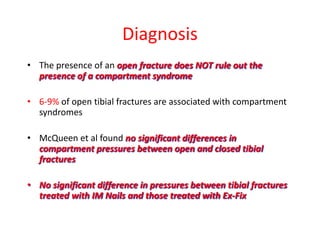
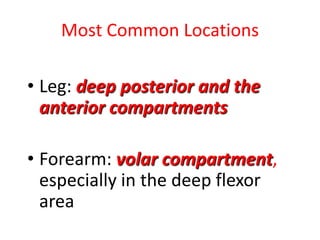
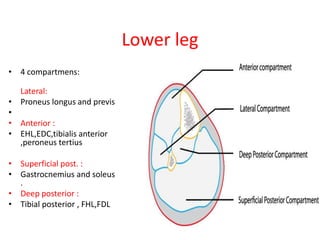
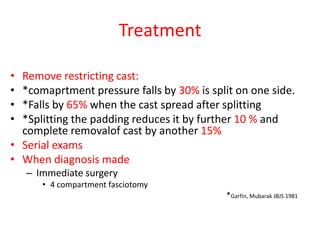
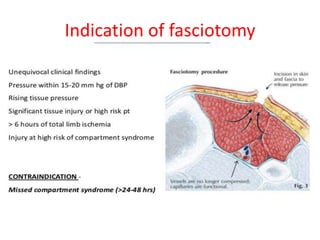
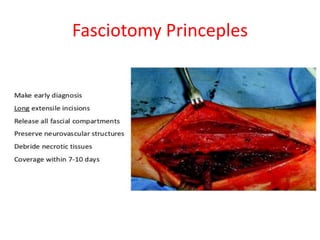
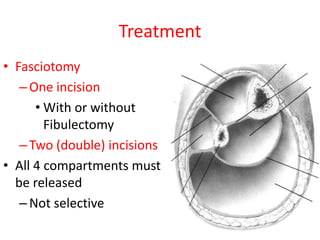
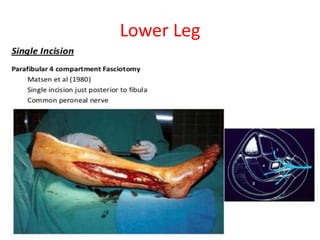
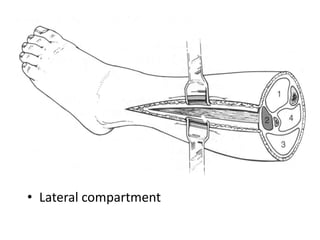
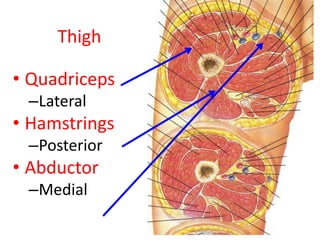
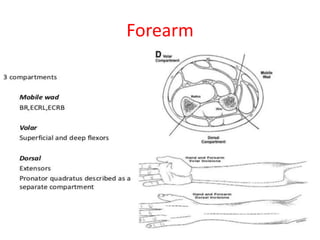
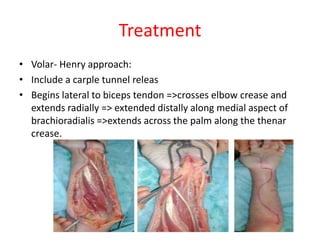
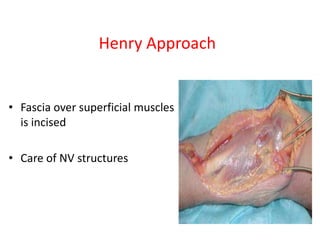
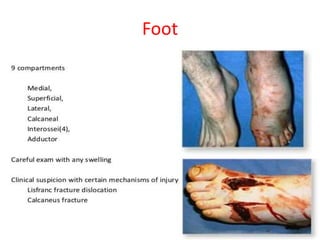
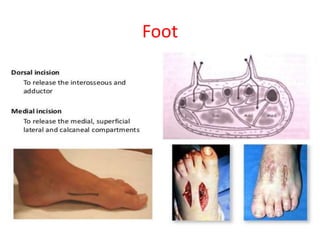
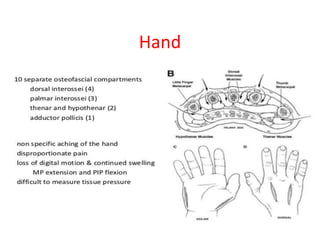
Compartment syndrome occurs when increased pressure within a closed osteofascial space compromises blood flow to muscles and nerves. It is most commonly caused by fractures that increase swelling. The diagnosis is based on pain disproportionate to the injury that worsens with passive stretching. While signs like pallor, paralysis and pulselessness occur late, an early fasciotomy is the definitive treatment to prevent permanent damage. Locations prone to compartment syndrome include the lower leg, forearm, thigh and foot.