This document provides information about compartment syndrome, including:
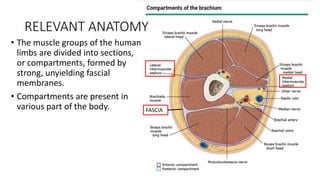
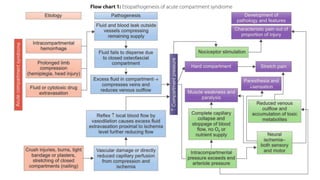
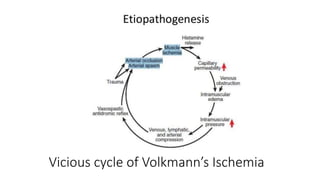
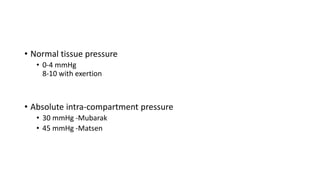
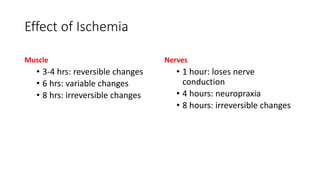
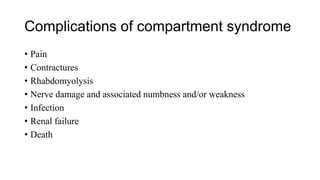
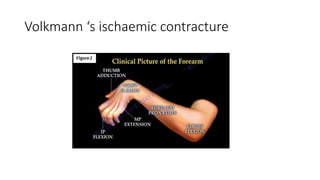
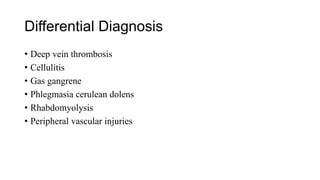
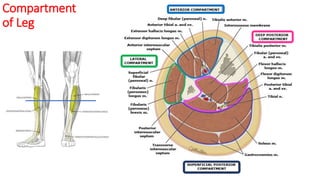
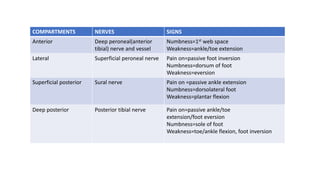
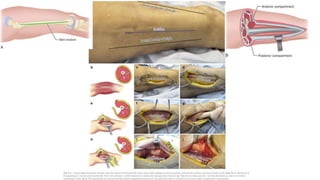
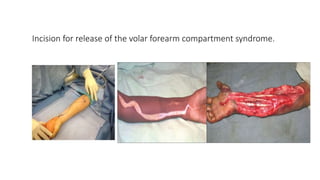
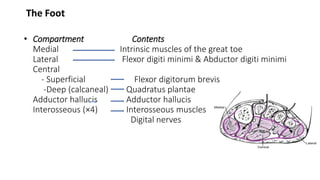
1. Compartment syndrome is defined as elevated pressure within a closed osteofascial compartment, compromising microcirculation. It commonly affects the leg and forearm.
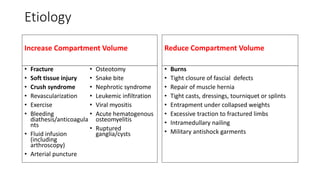
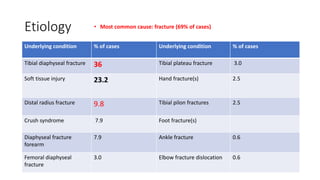
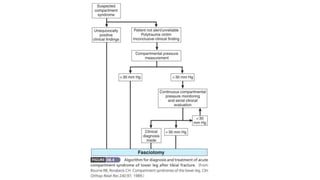
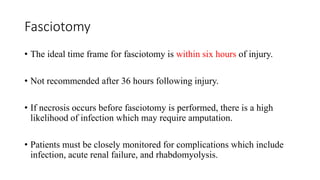
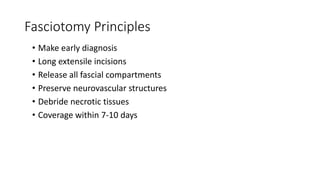
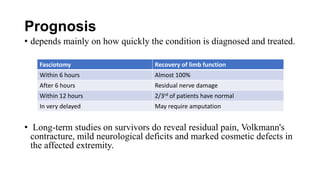
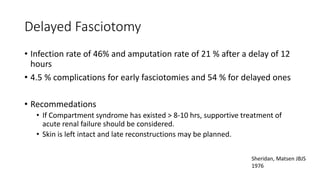
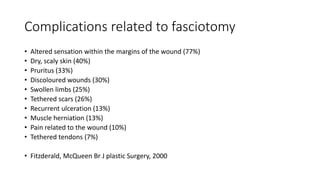
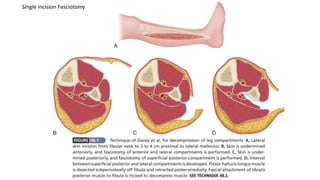
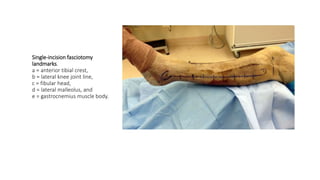
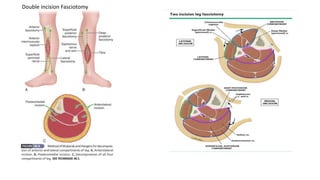
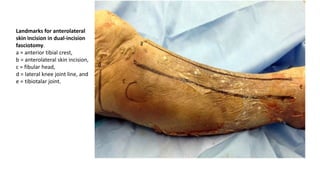
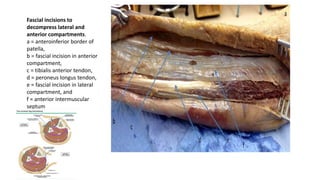
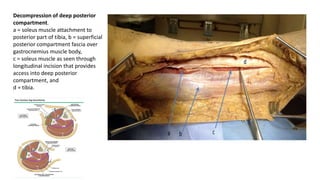
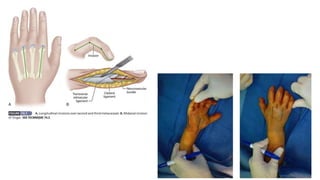
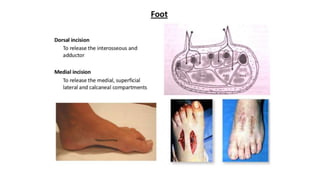
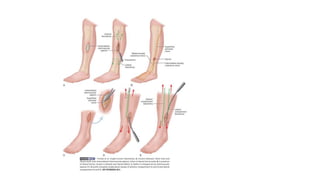
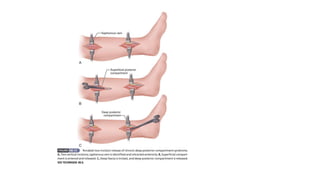
2. Causes include fractures, crush injuries, reperfusion, and tight dressings. Acute compartment syndrome requires prompt diagnosis and fasciotomy within 6 hours for best outcomes.
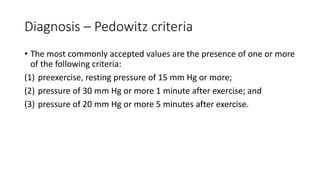
3. Chronic exertional compartment syndrome involves reversible ischemia in noncompliant compartments unresponsive to exercise-induced swelling. It typically causes exercise-induced leg pain resolving with rest.









![References
• Campbell’s Operative Orthopaedics 4th Edition
• J. Maheshwari 5th Edition
• Apley’s 9th Edition
• UpToDate Version 3.0
• Torlincasi AM, Lopez RA, Waseem M. Acute Compartment Syndrome.
[Updated 2021 Feb 10]. In: StatPearls [Internet]. Treasure Island (FL):
StatPearls Publishing; 2021 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK448124/](https://image.slidesharecdn.com/compartmentsyndrome-210930141041/85/Compartment-syndrome-77-320.jpg)
