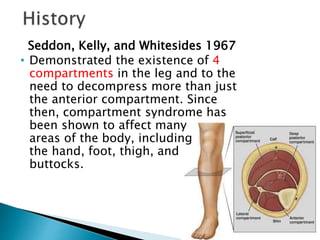
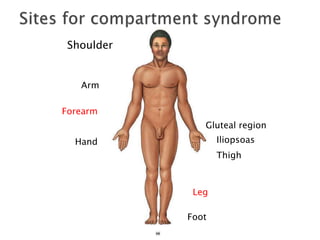
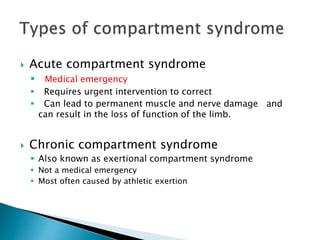
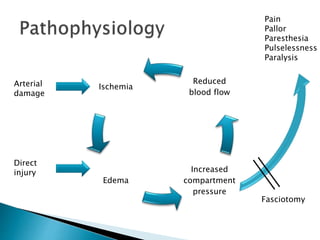
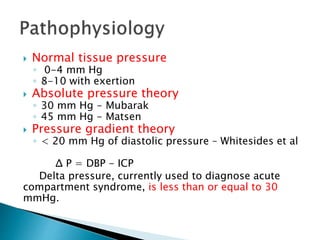
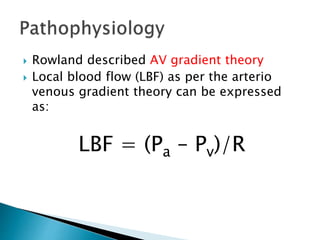
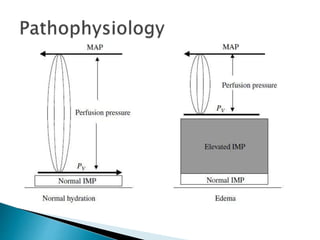
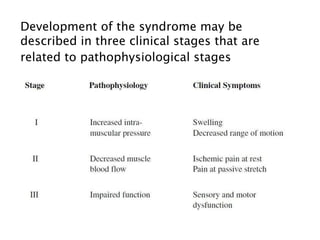
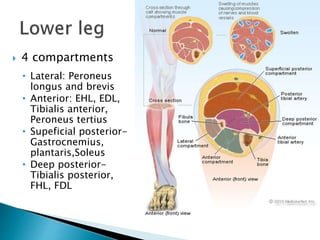
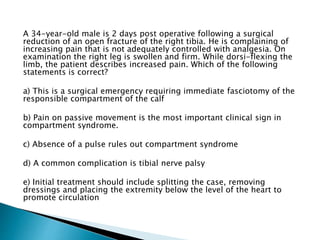
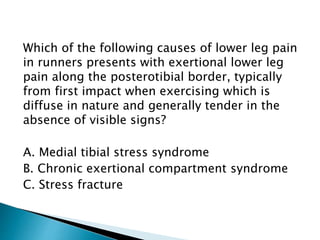
This document discusses the history, pathophysiology, diagnosis, and management of compartment syndrome. It notes that compartment syndrome is characterized by increased tissue pressure within a closed anatomical space that compromises circulation and function. Key points include:
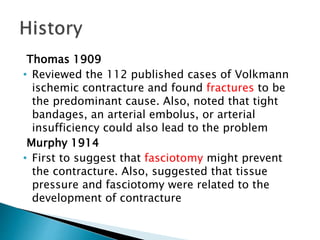
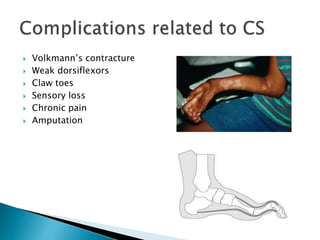
- Compartment syndrome was first described by Richard von Volkmann in 1881 and the term was coined by Hildebrand in 1906.
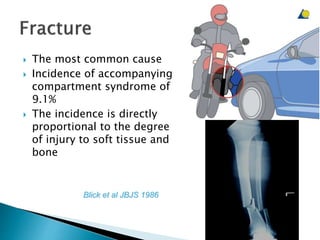
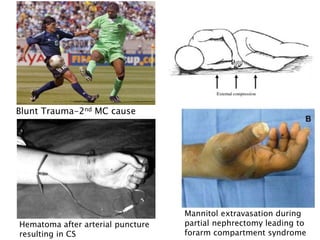
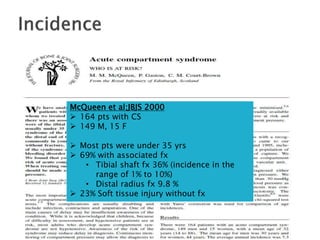
- The most common causes are fractures and soft tissue injuries, which can lead to bleeding inside an anatomical compartment.
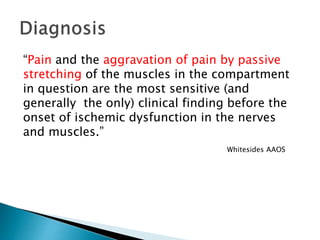
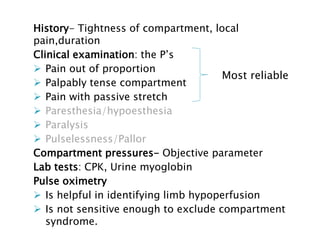
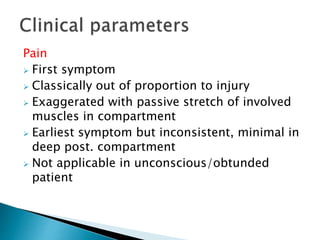
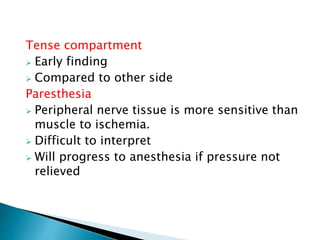
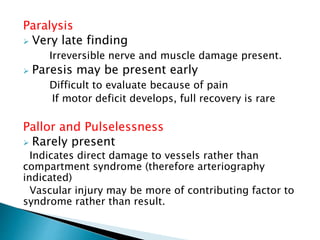
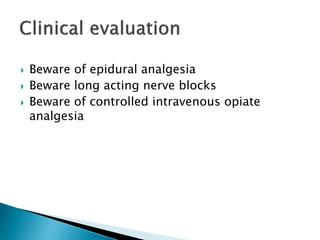
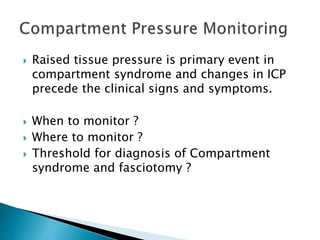
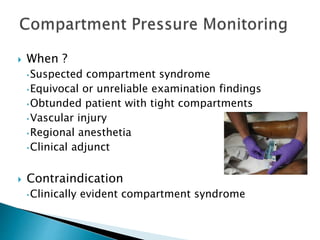
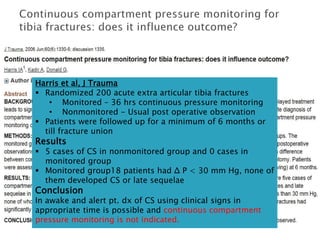
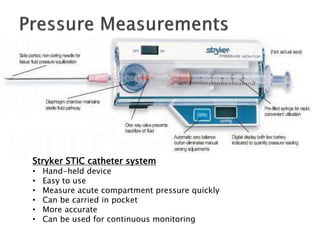
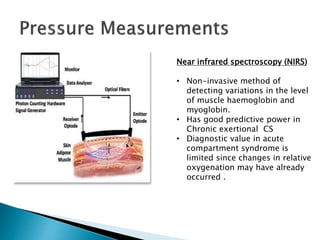
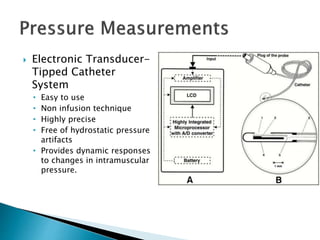
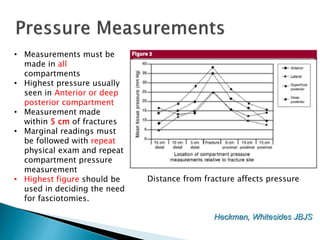
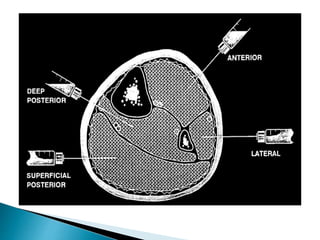
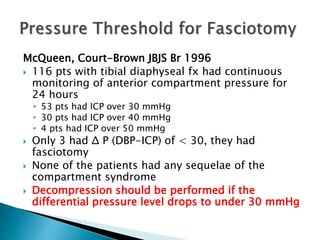
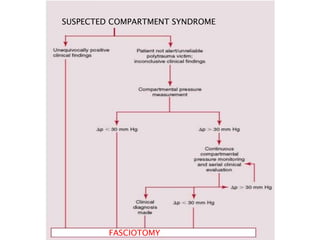
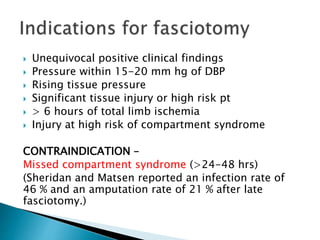
- Diagnosis involves evaluating the patient for pain out of proportion, tense compartments, sensory changes, and measuring compartment pressure.
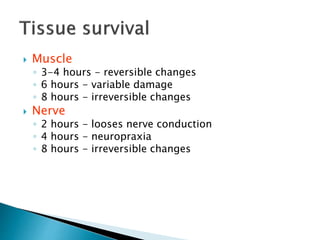
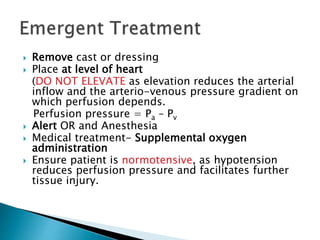
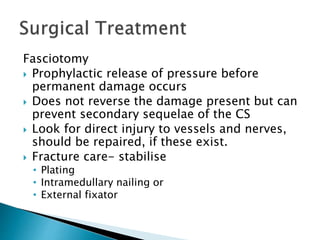
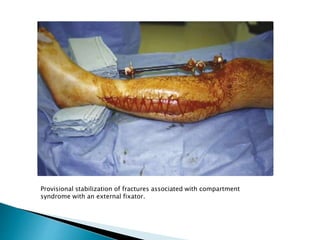
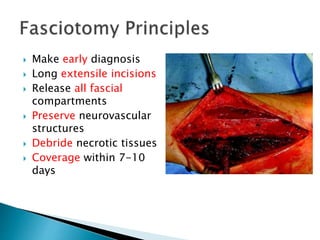
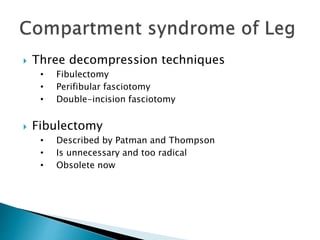
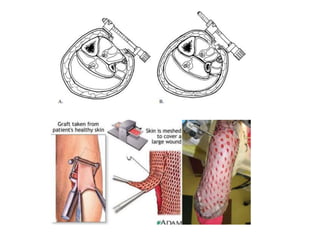
- Untreated, it can lead to permanent muscle and nerve damage within hours; fasciotomy is