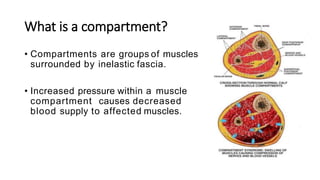
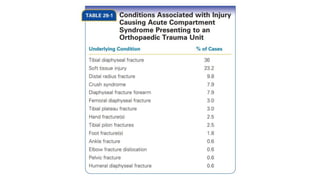
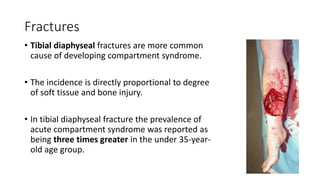
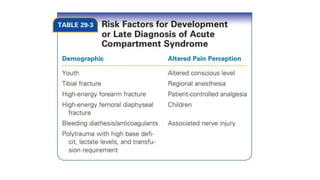
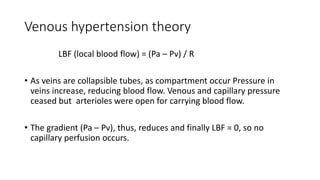
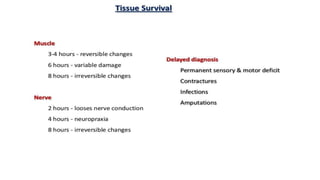
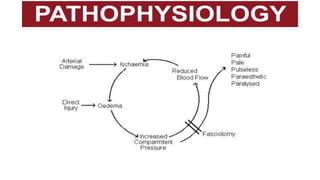
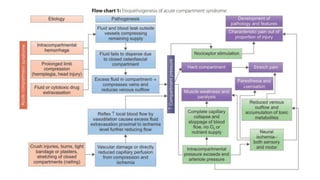
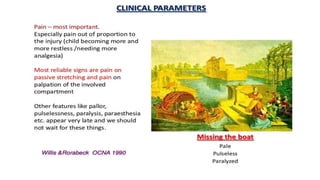
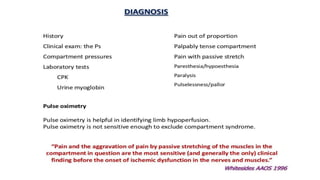
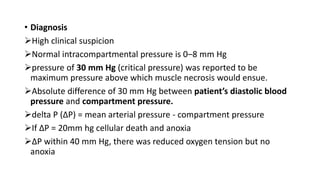
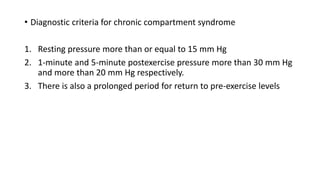
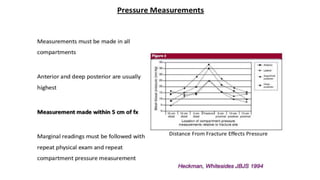
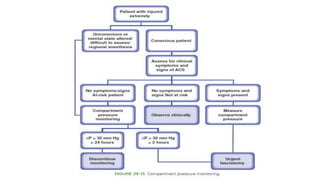
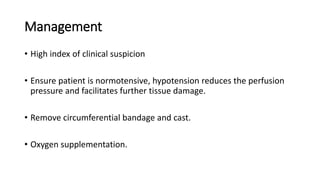
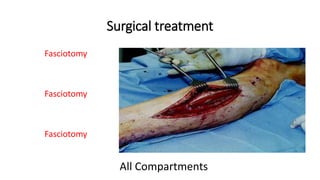
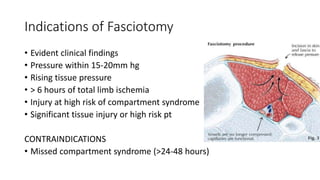
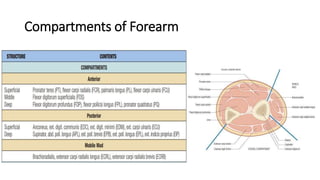
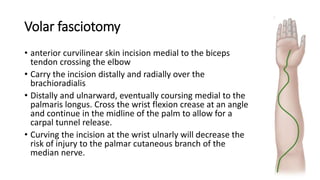
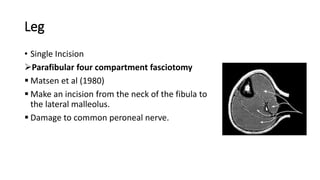
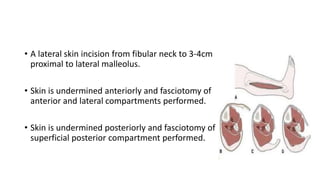
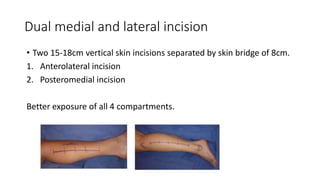
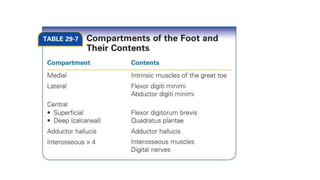
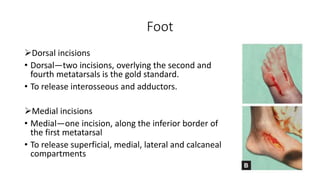
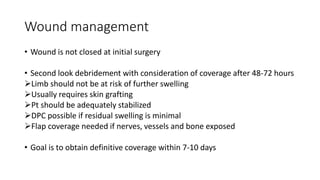
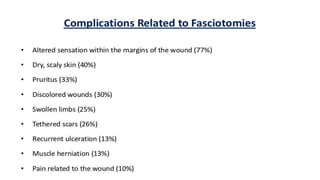
This document provides information on compartment syndrome, including its causes, signs and symptoms, diagnosis, and management. Compartment syndrome occurs when increased pressure within a muscle compartment compromises blood circulation. It can result from trauma, bleeding, or other injuries that cause swelling. Left untreated, it leads to muscle and nerve necrosis. Key signs are pain out of proportion to the injury and pain with passive stretching of the affected area. Treatment involves promptly performing fasciotomies to release the fascial compartments and restore blood flow. Early diagnosis and surgical decompression are important to prevent permanent tissue damage.