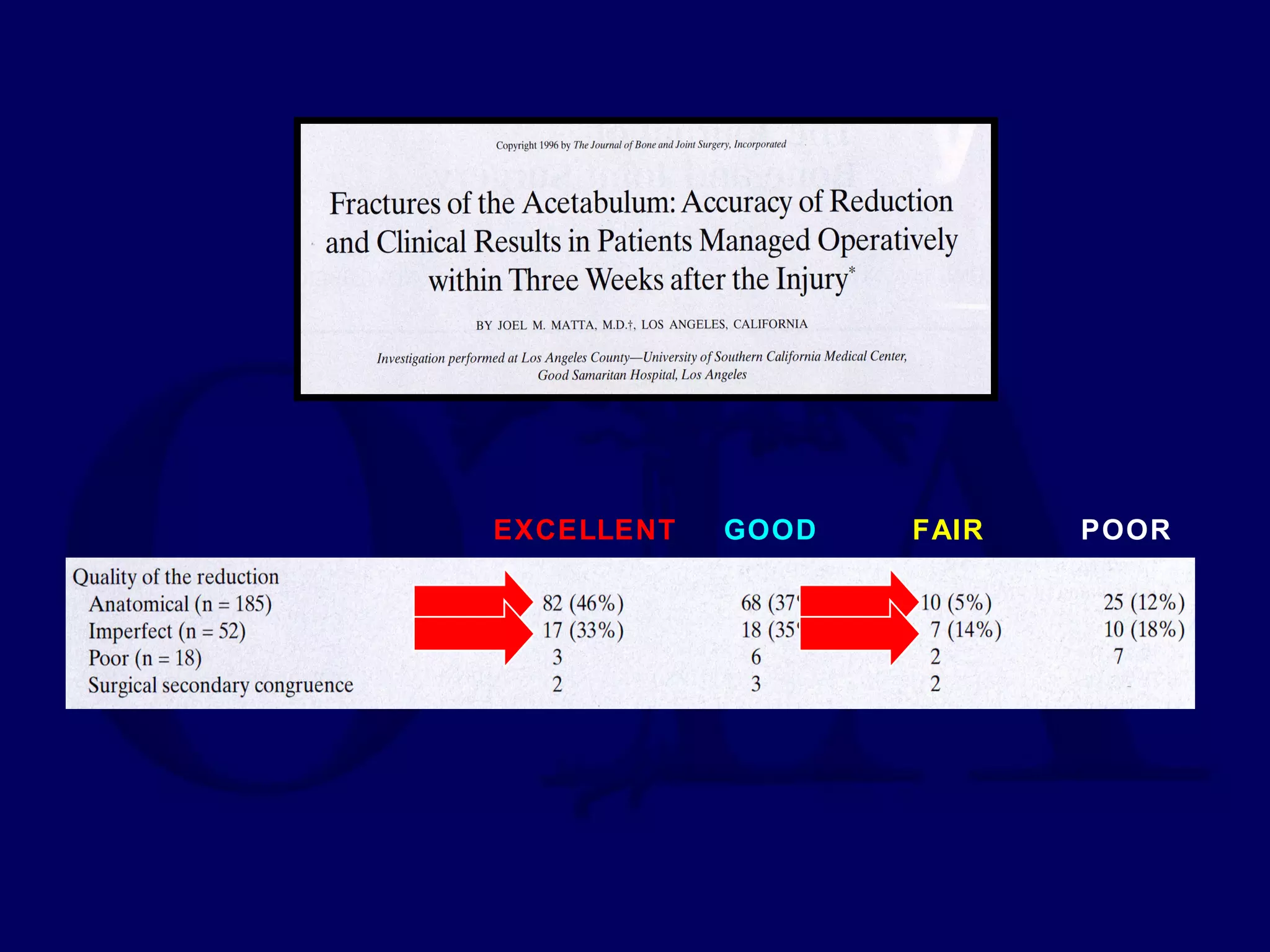
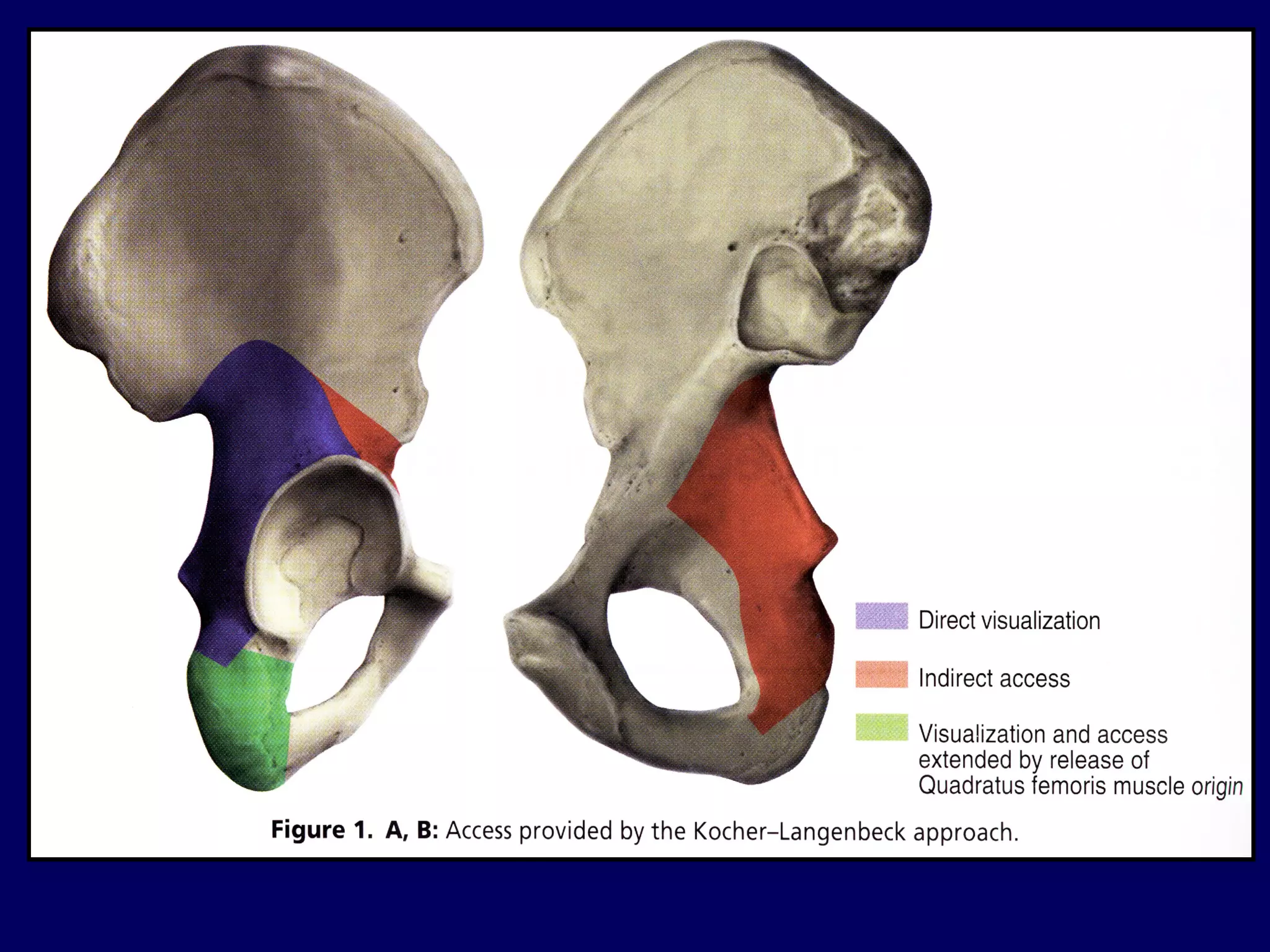
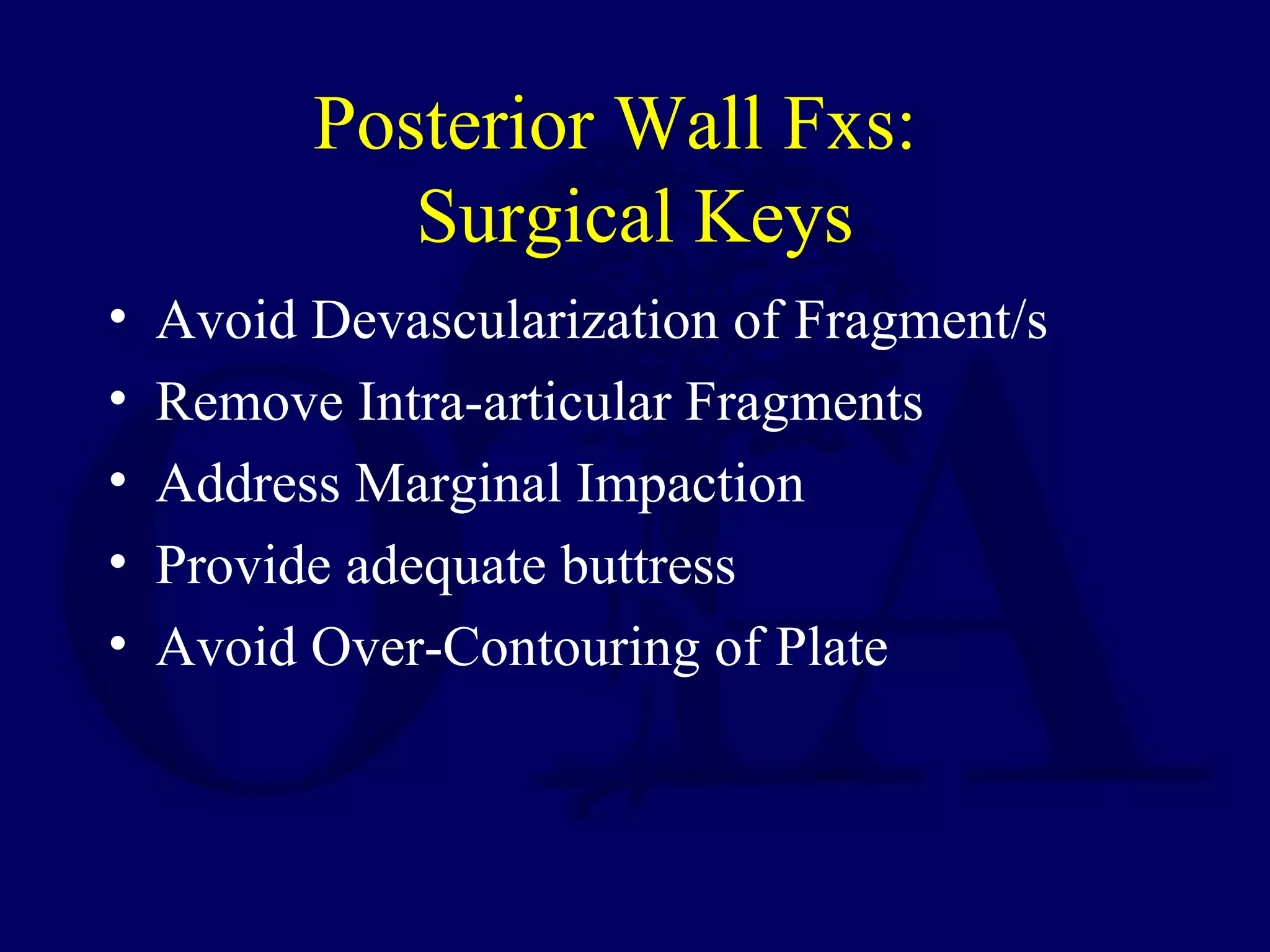
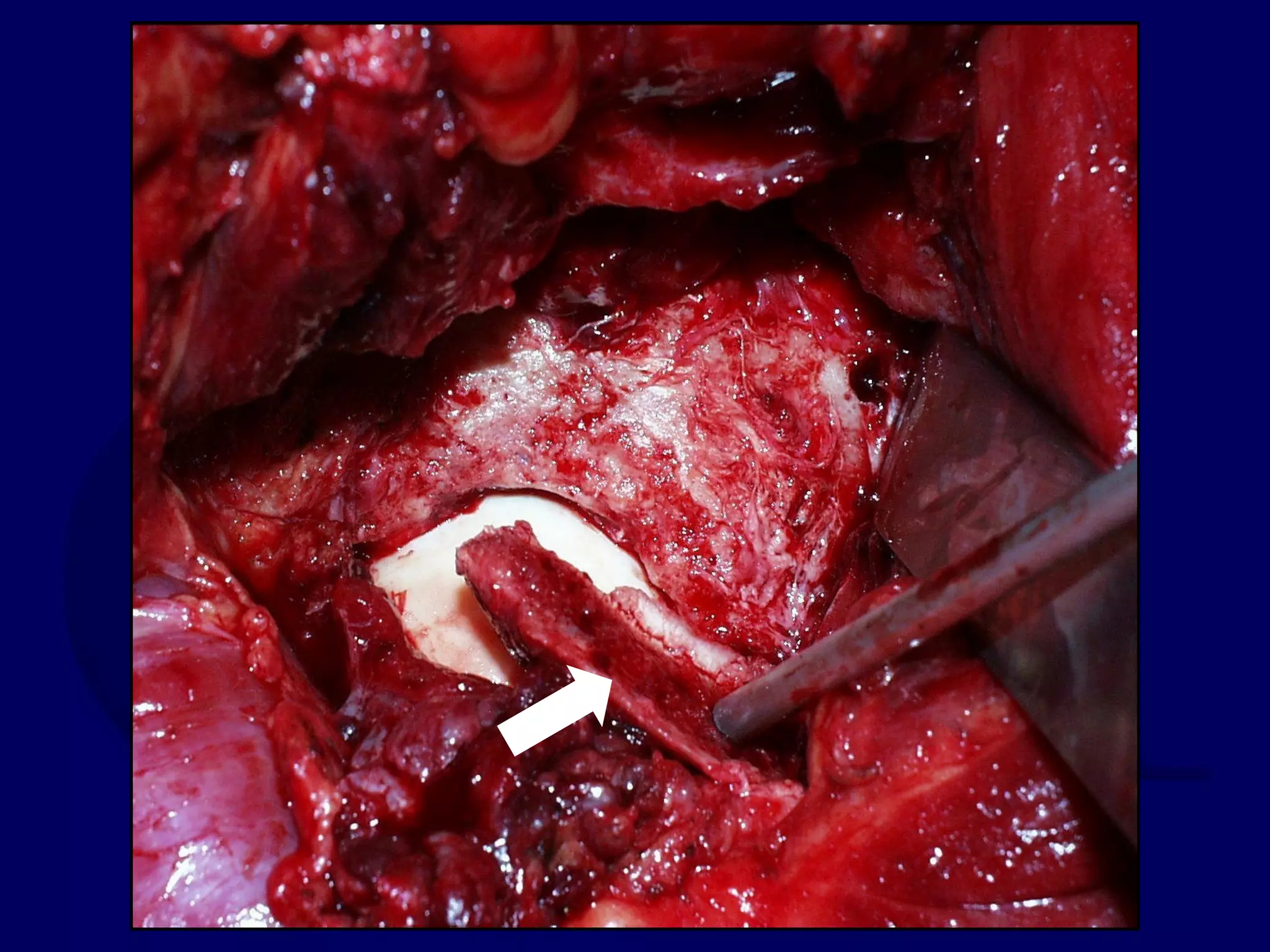
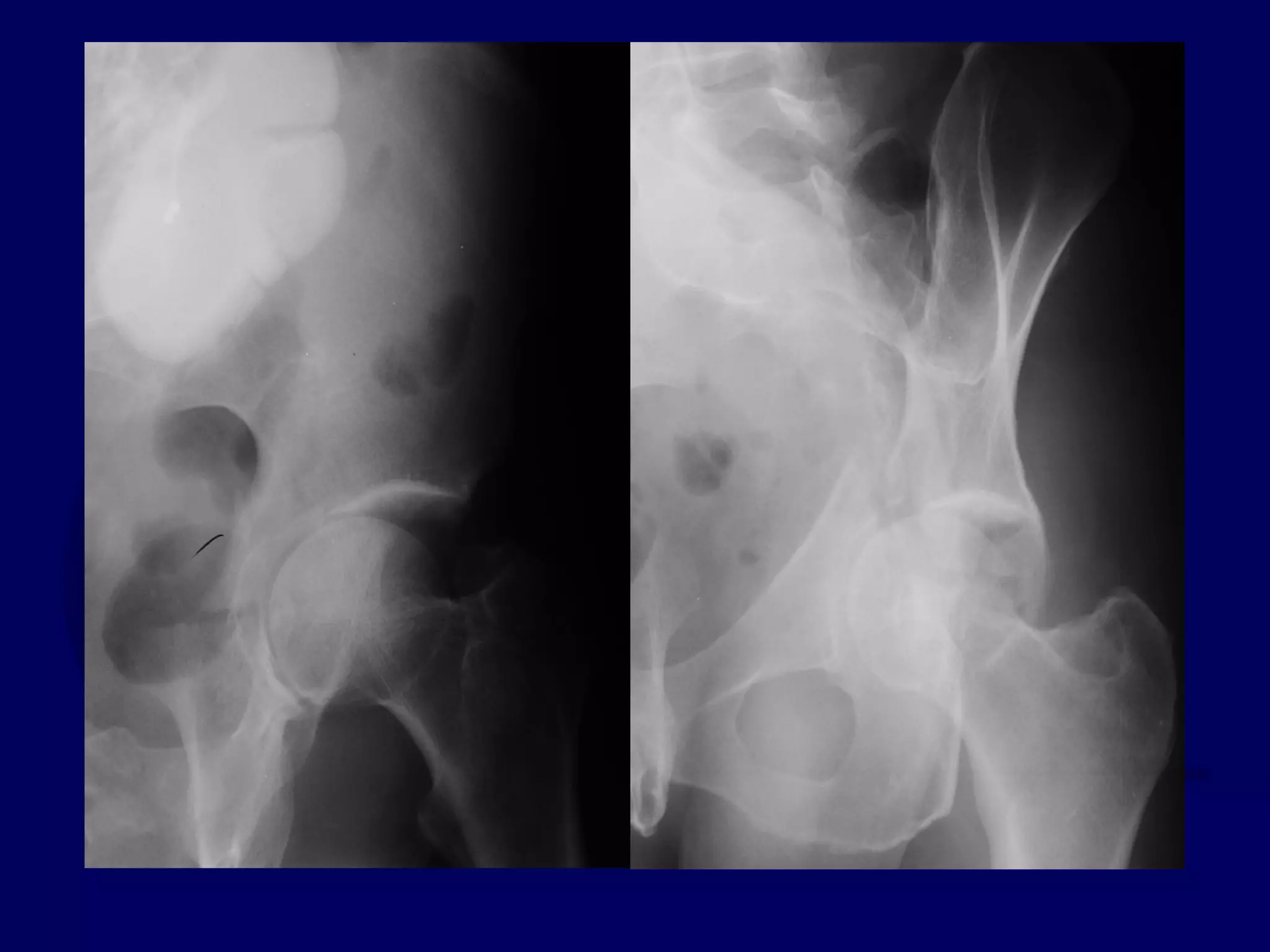
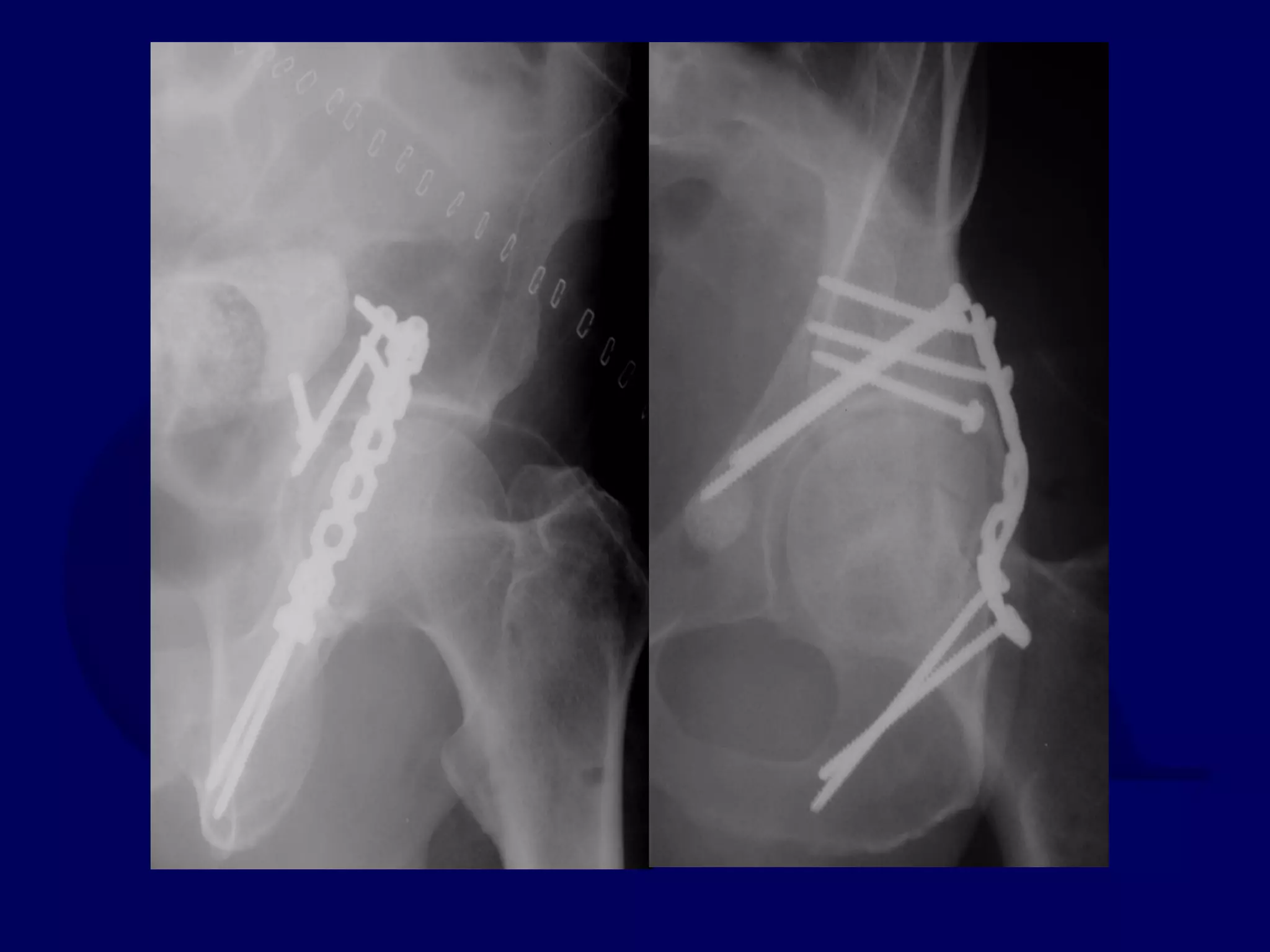
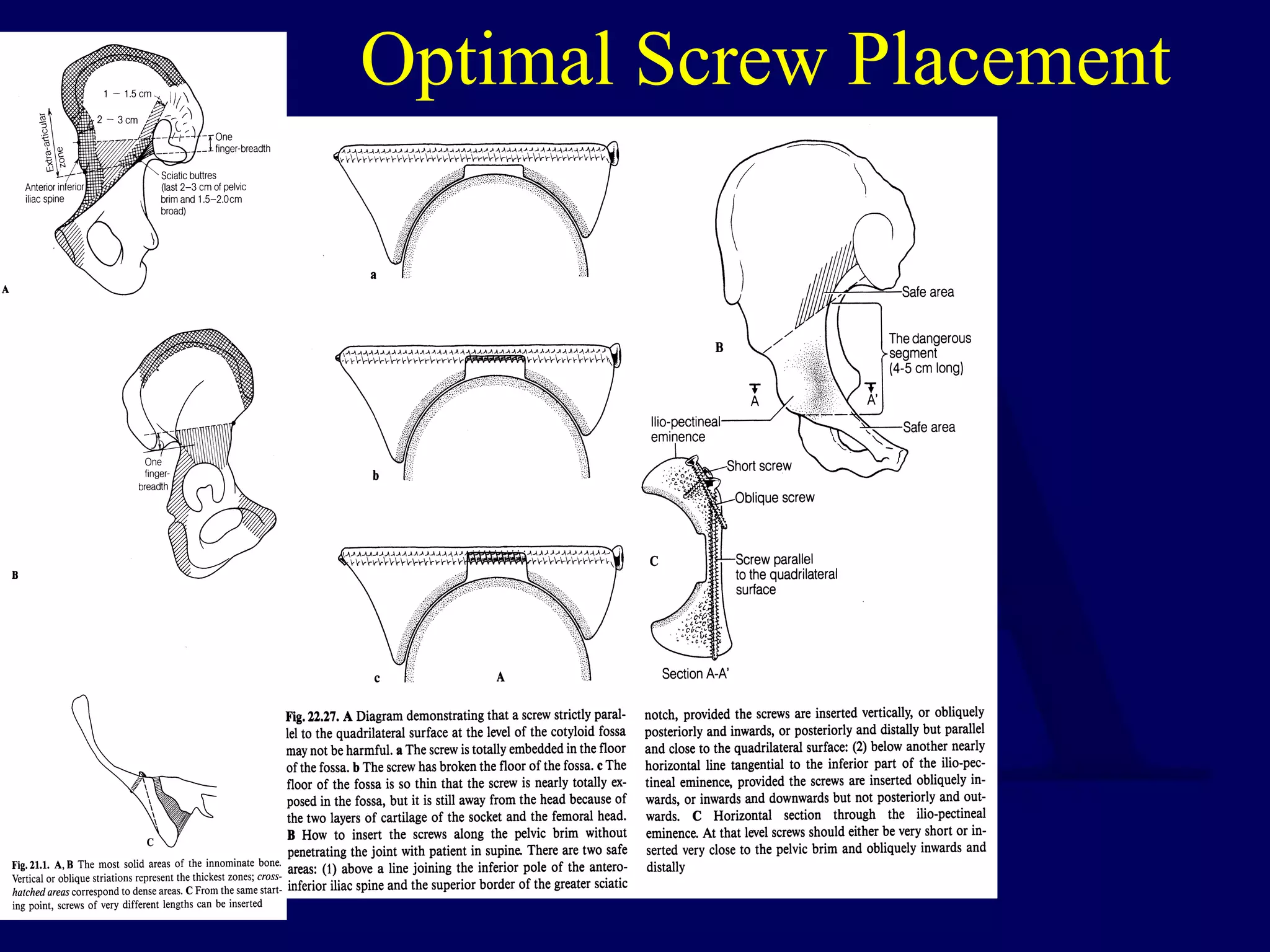
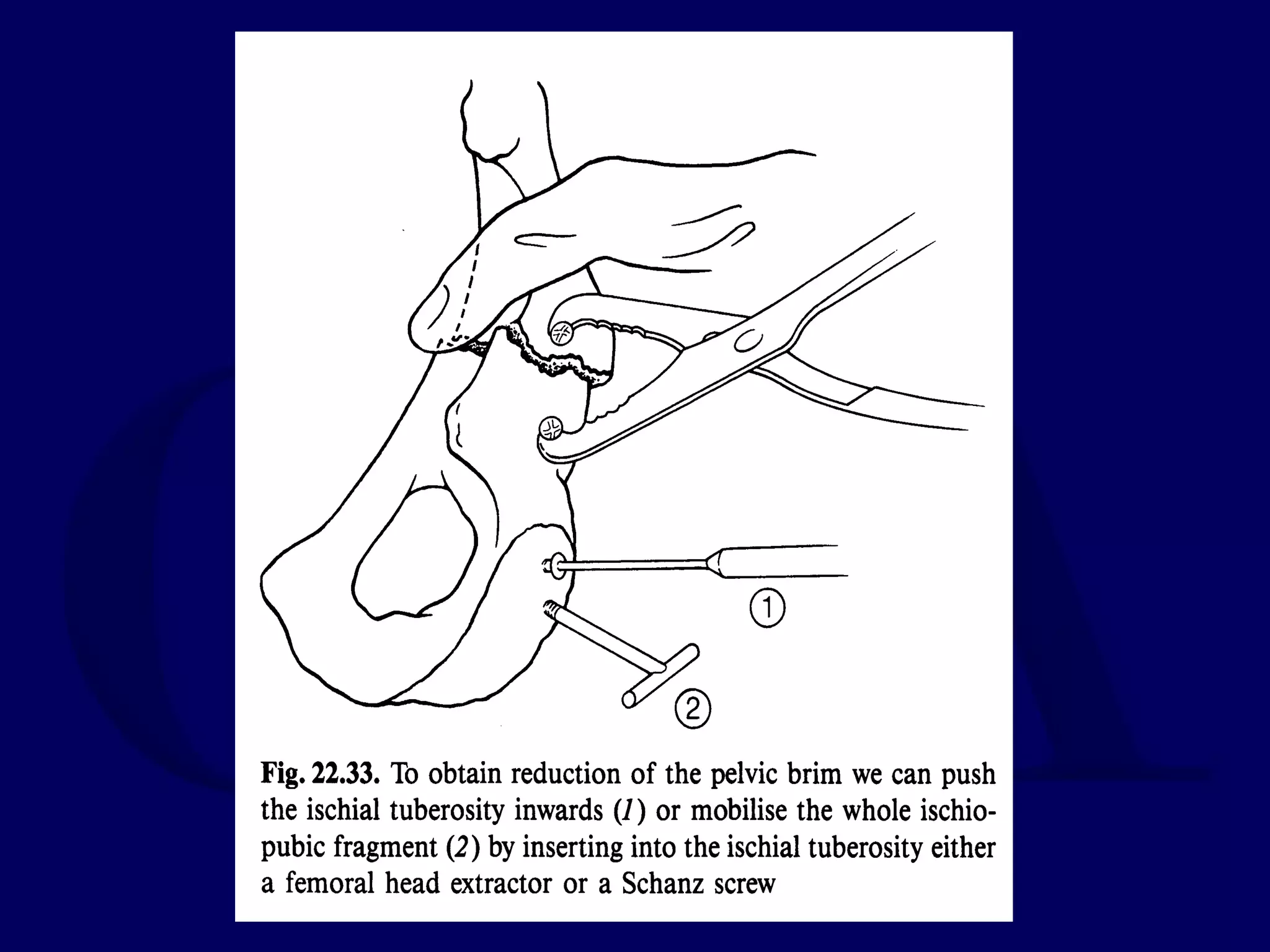
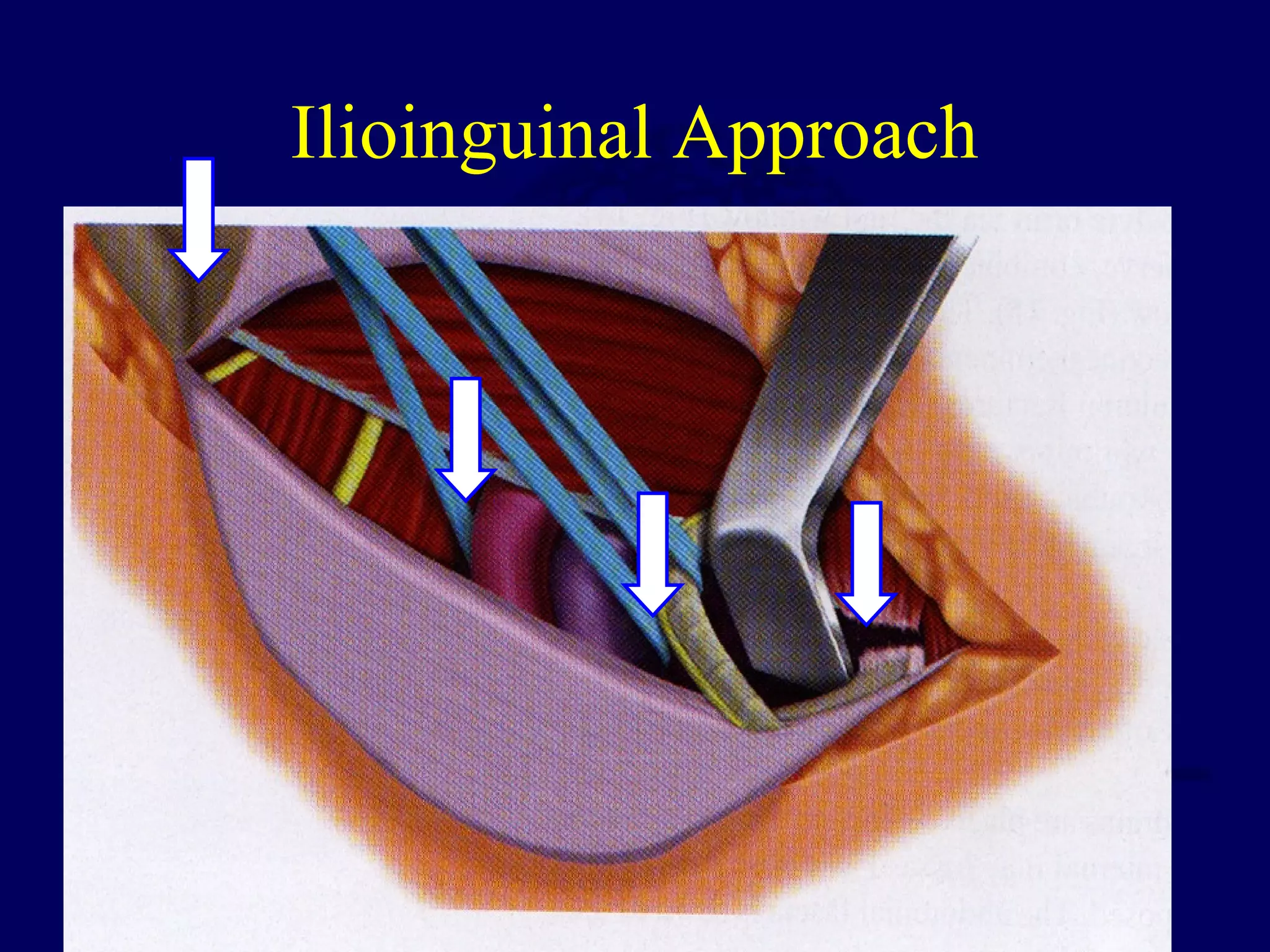
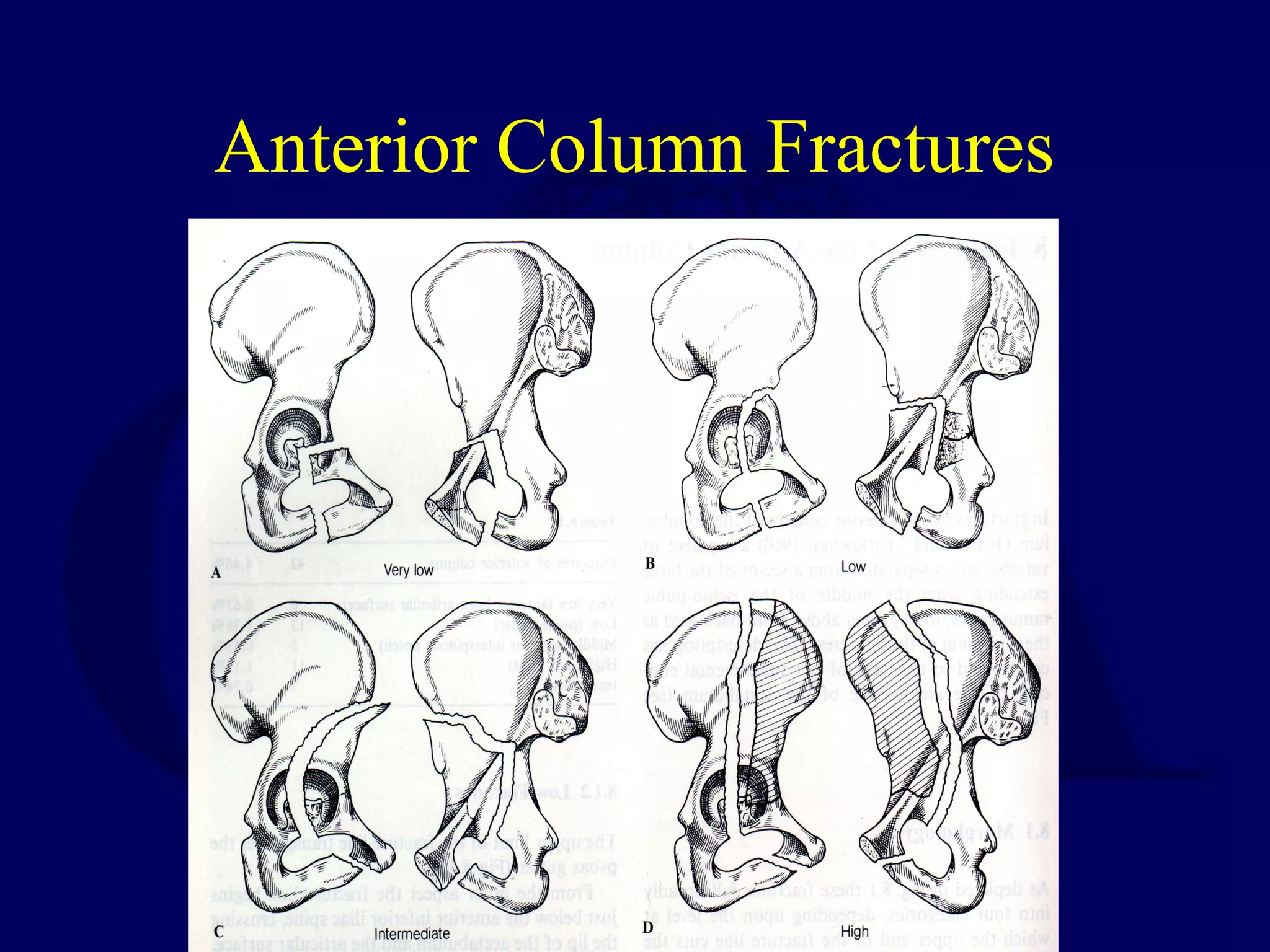
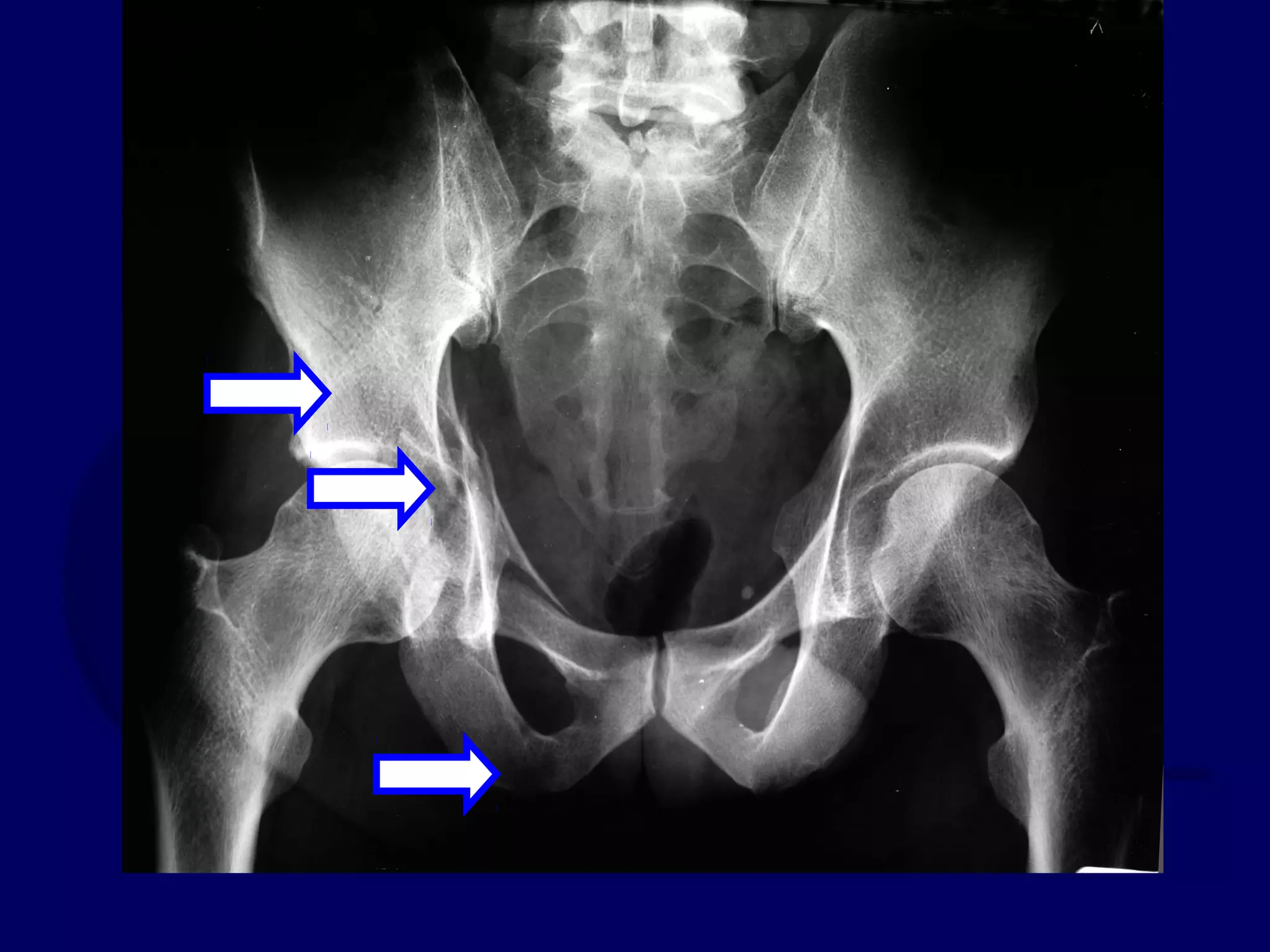
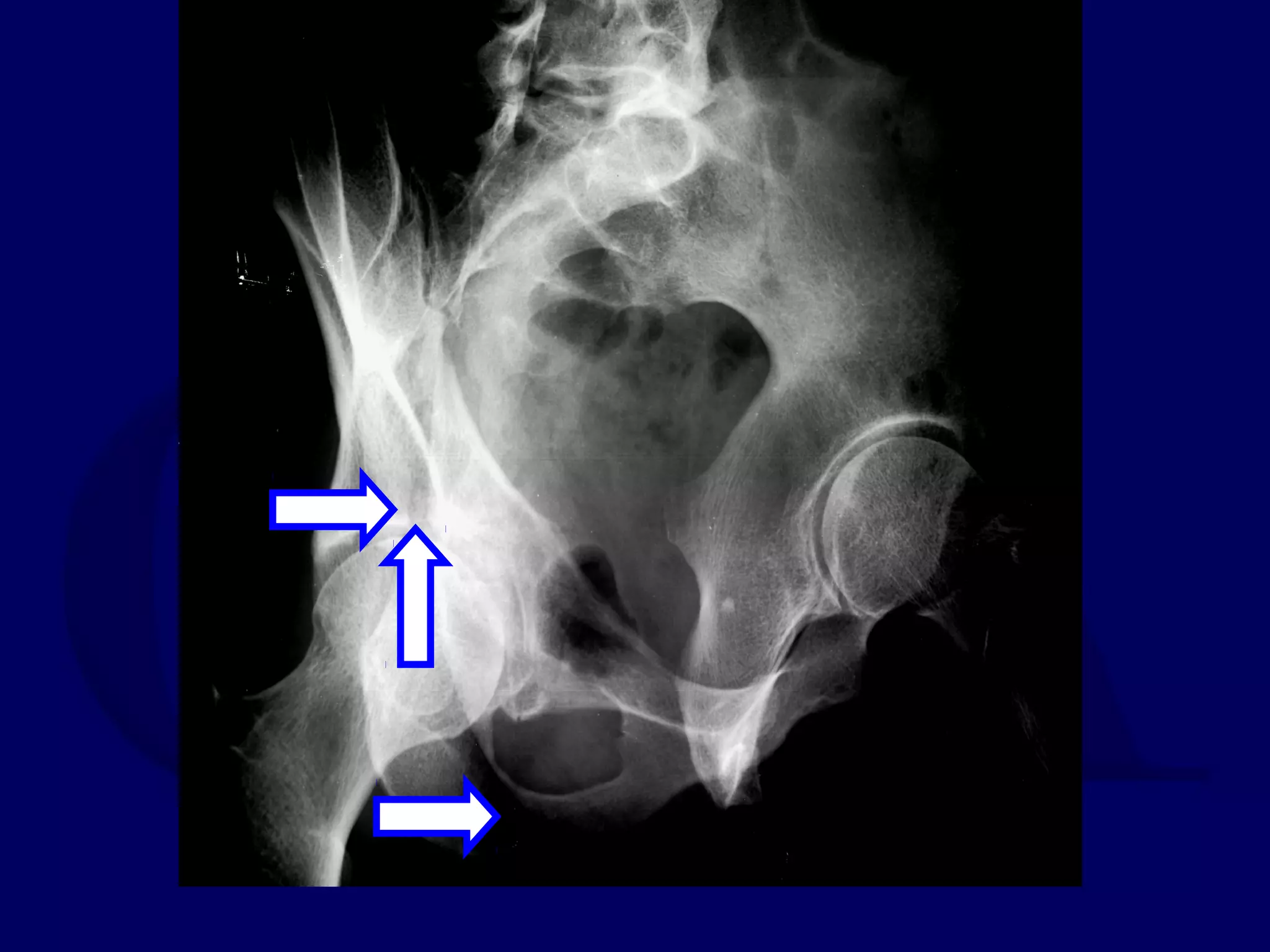
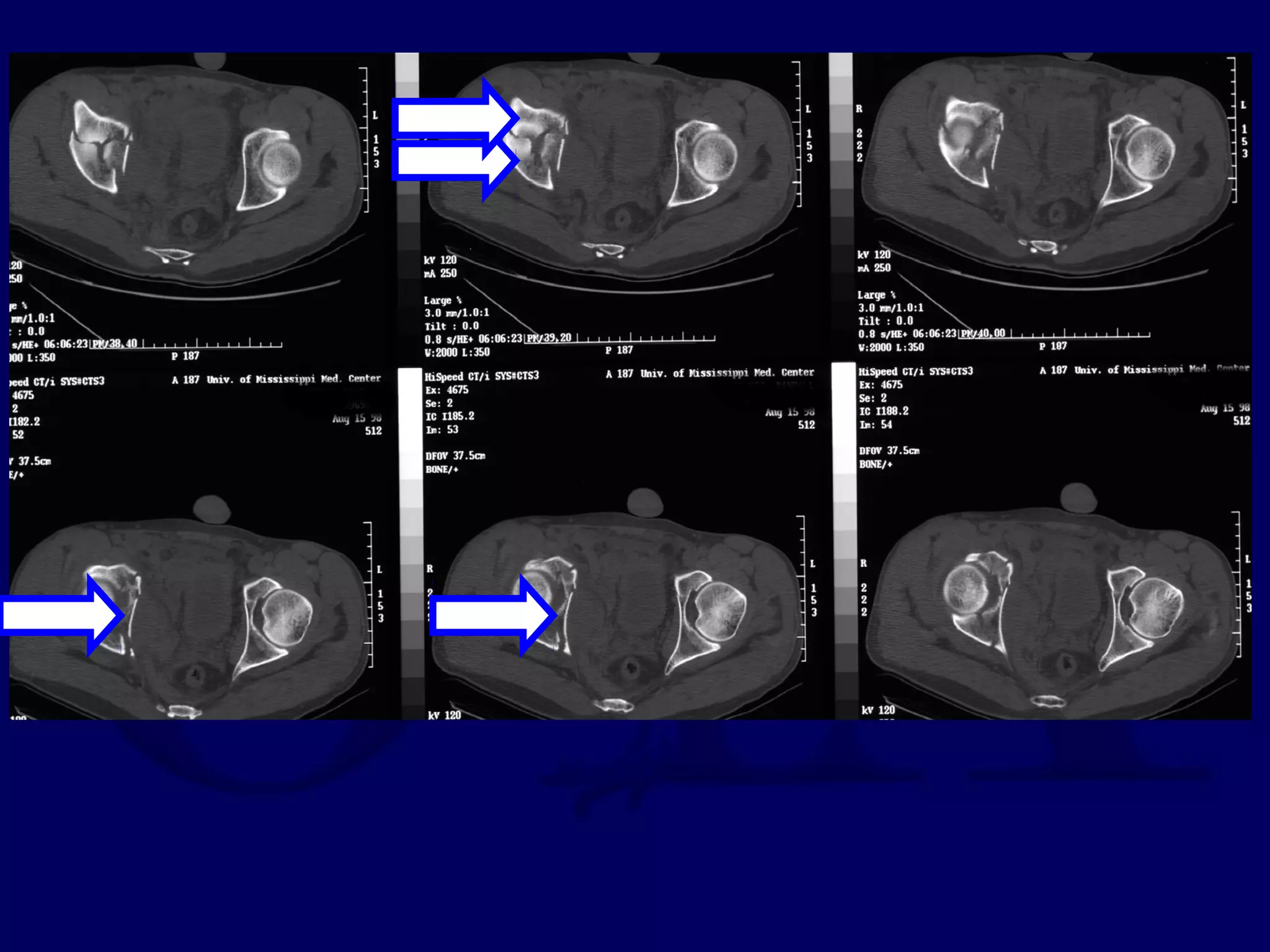
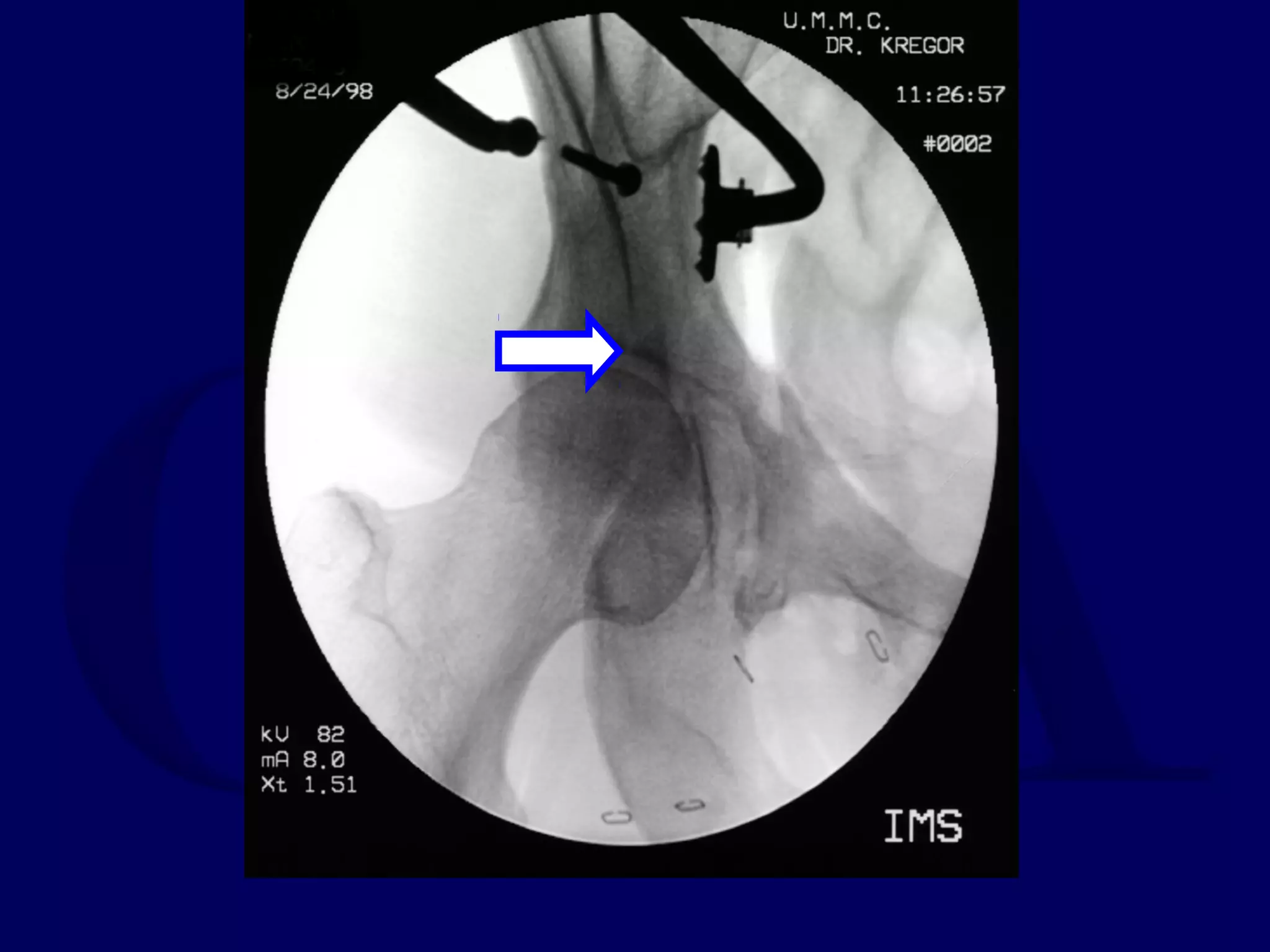
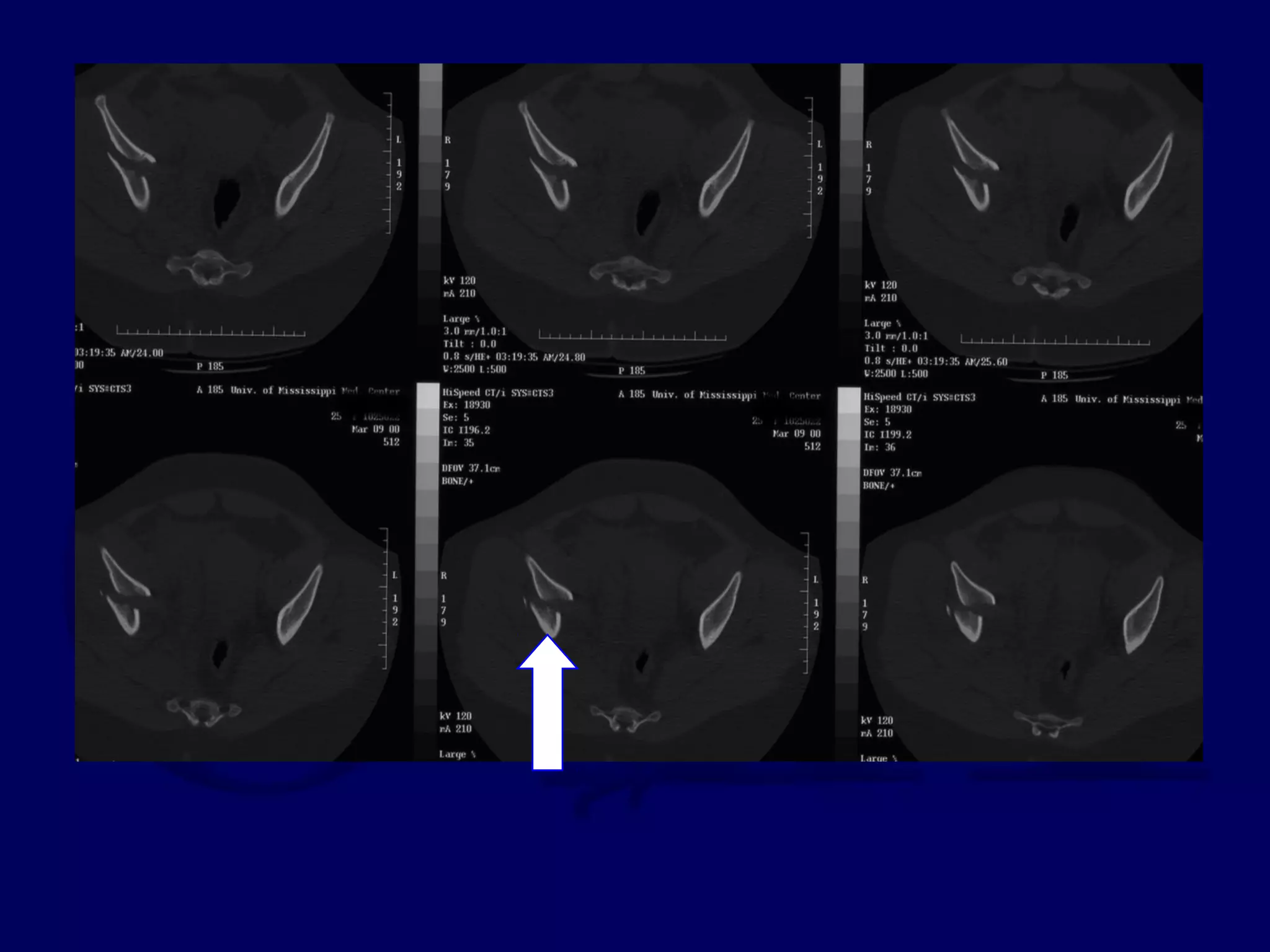
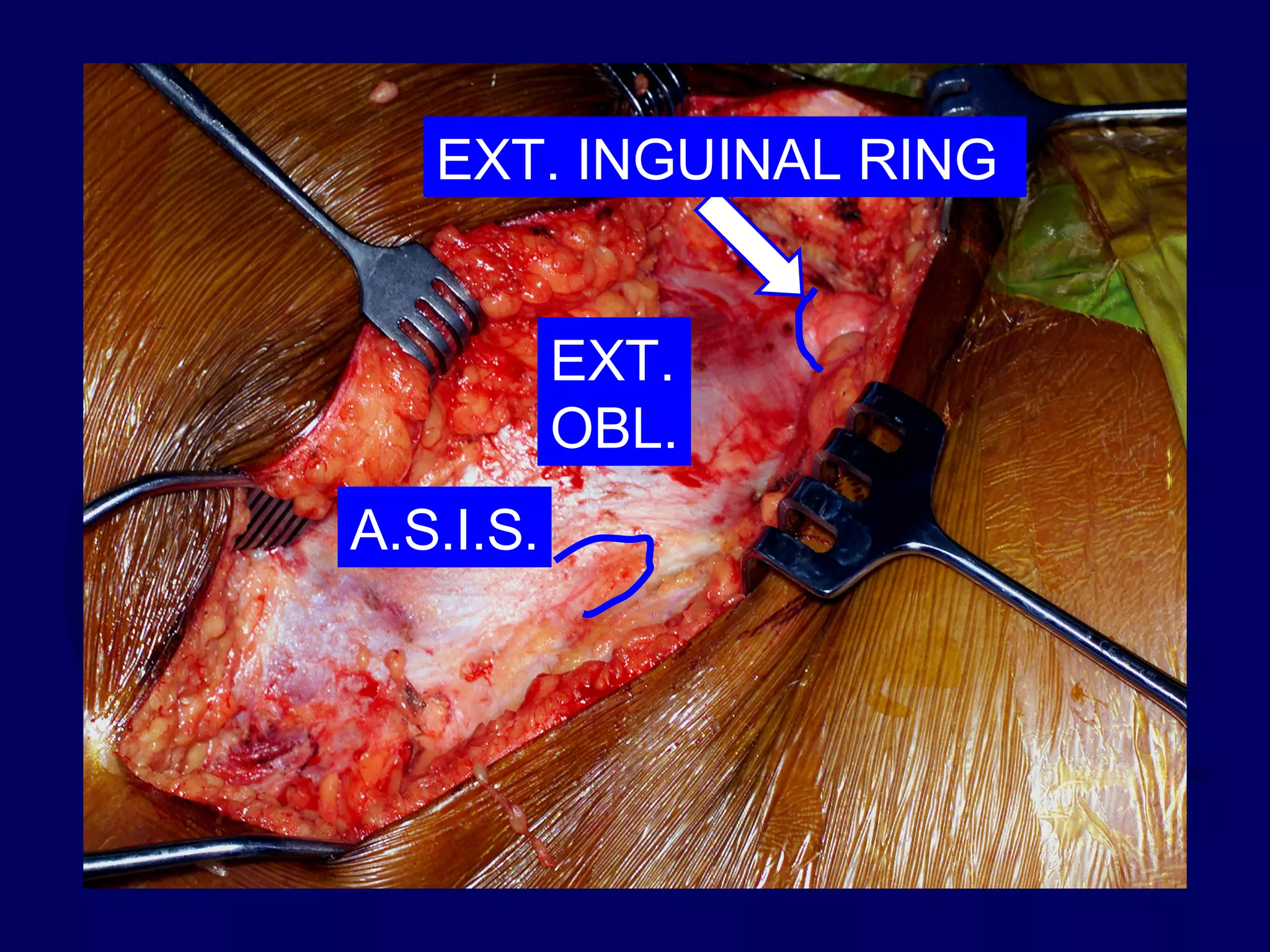
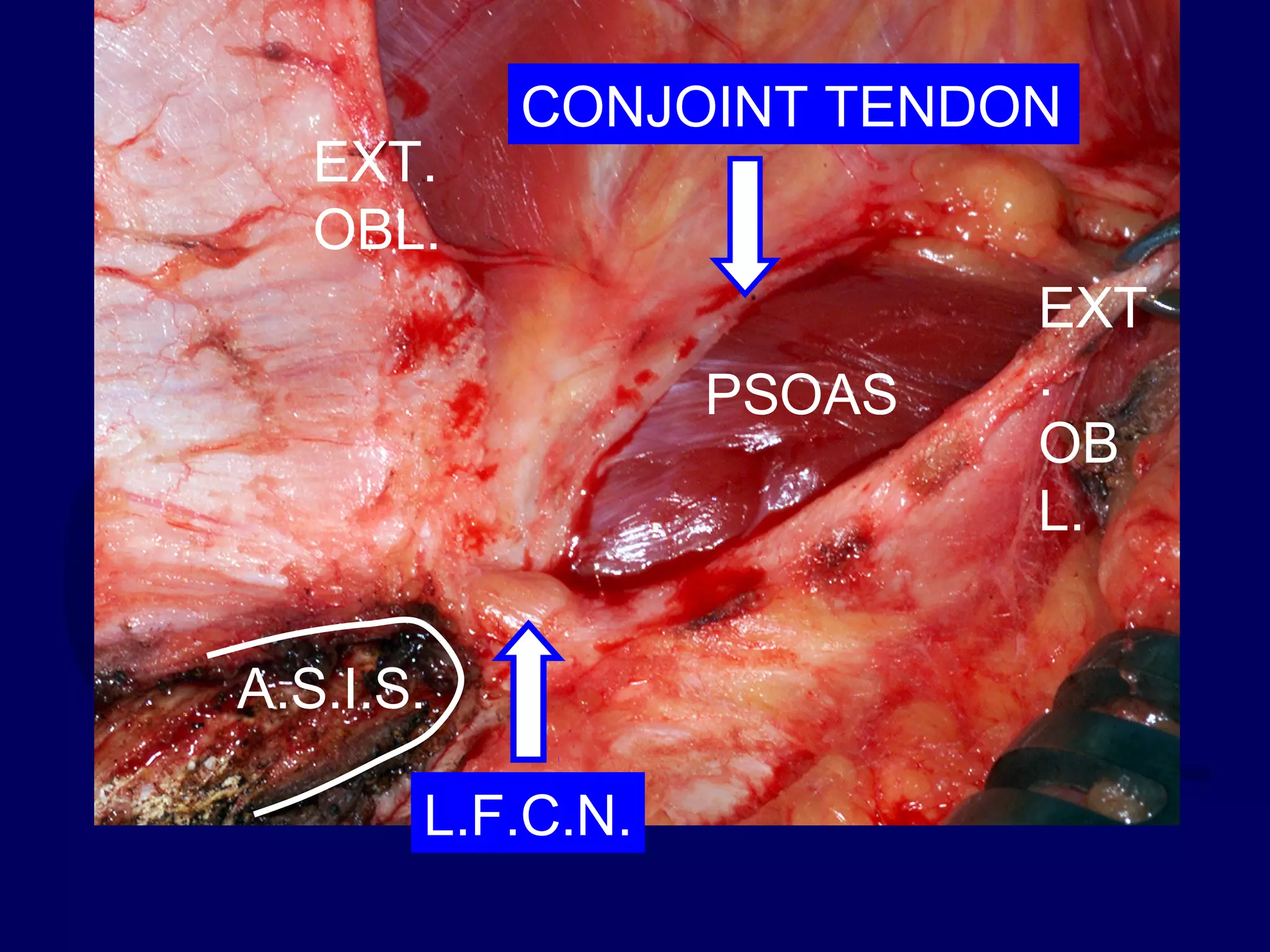
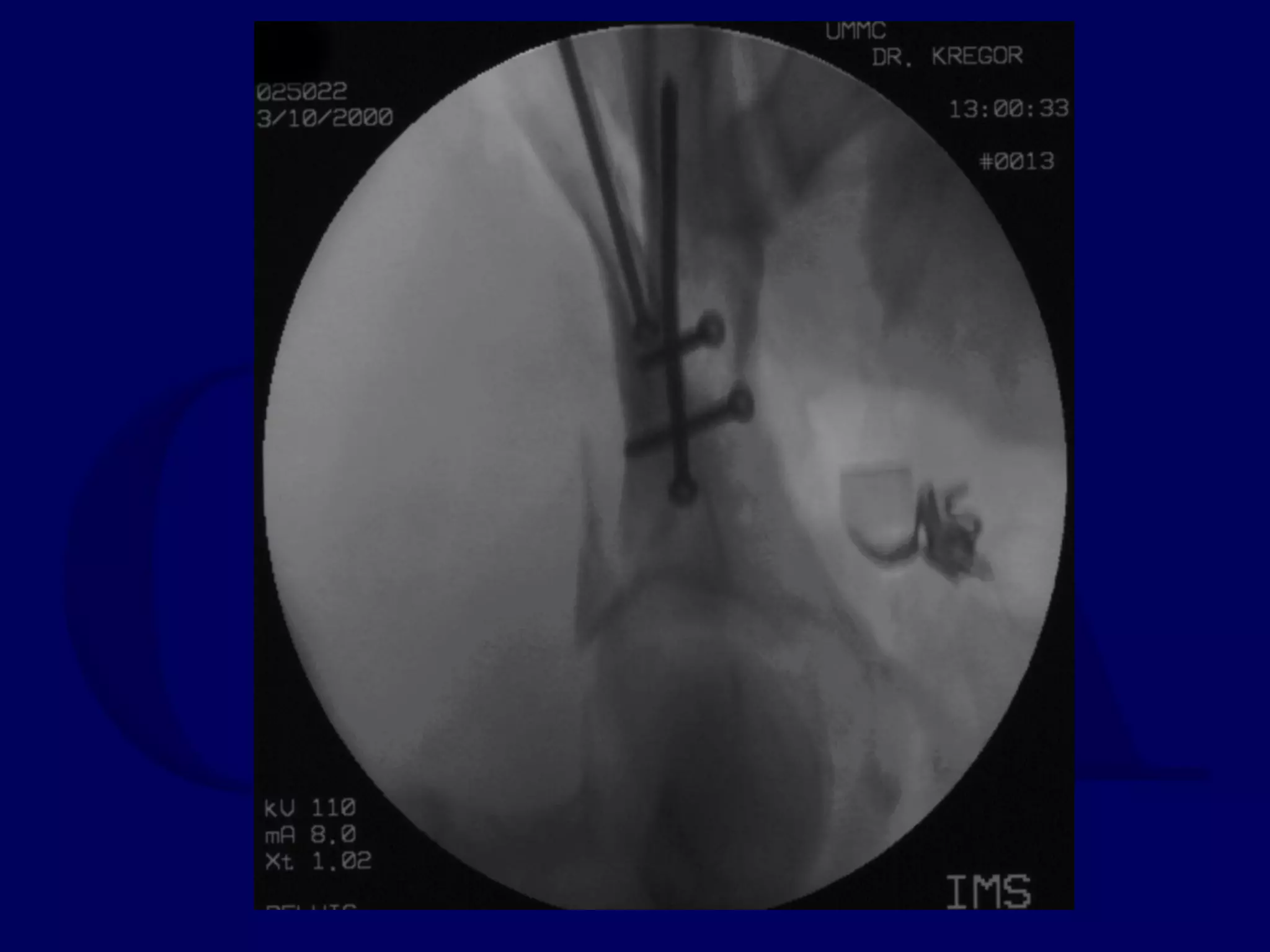
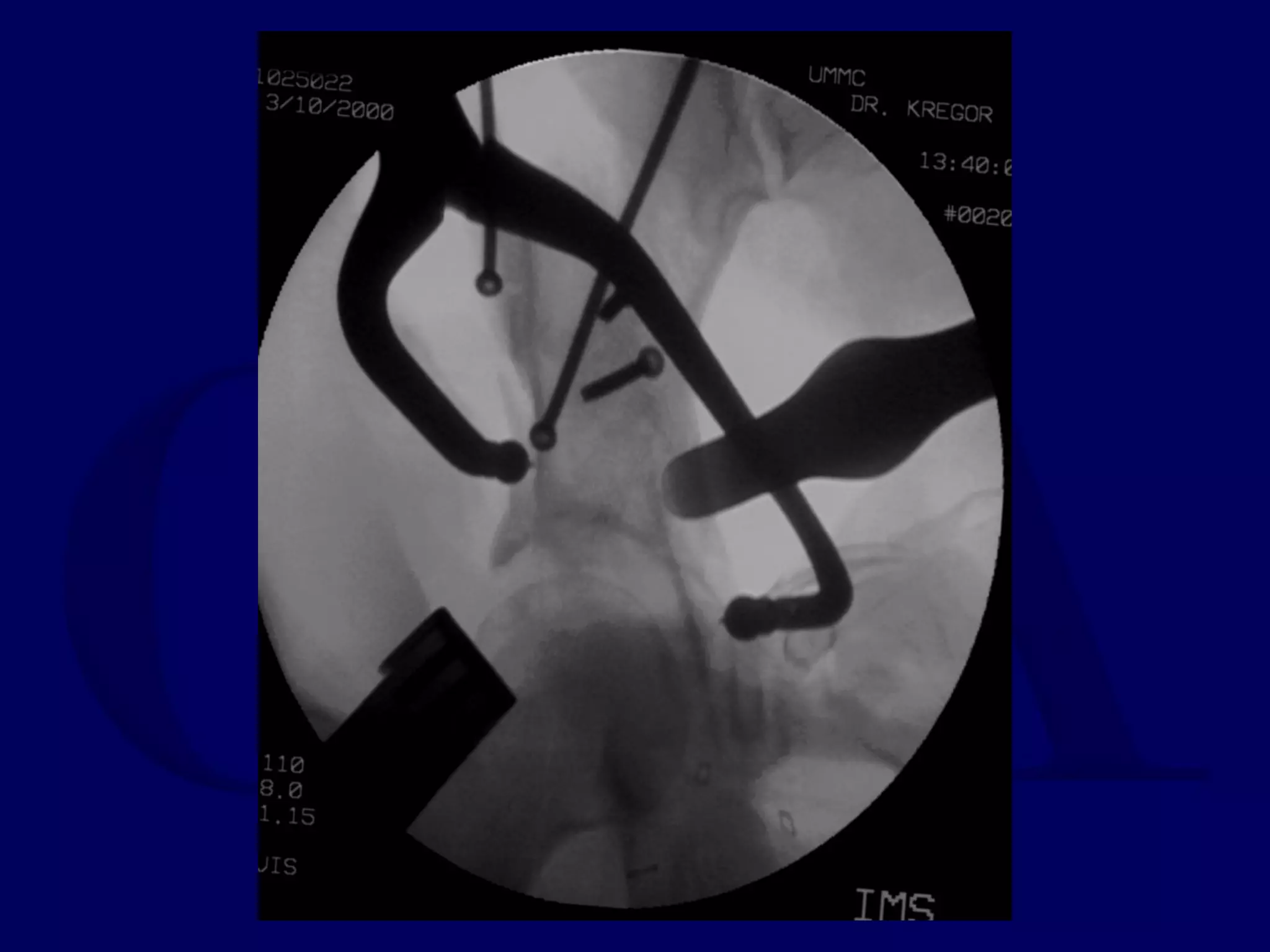
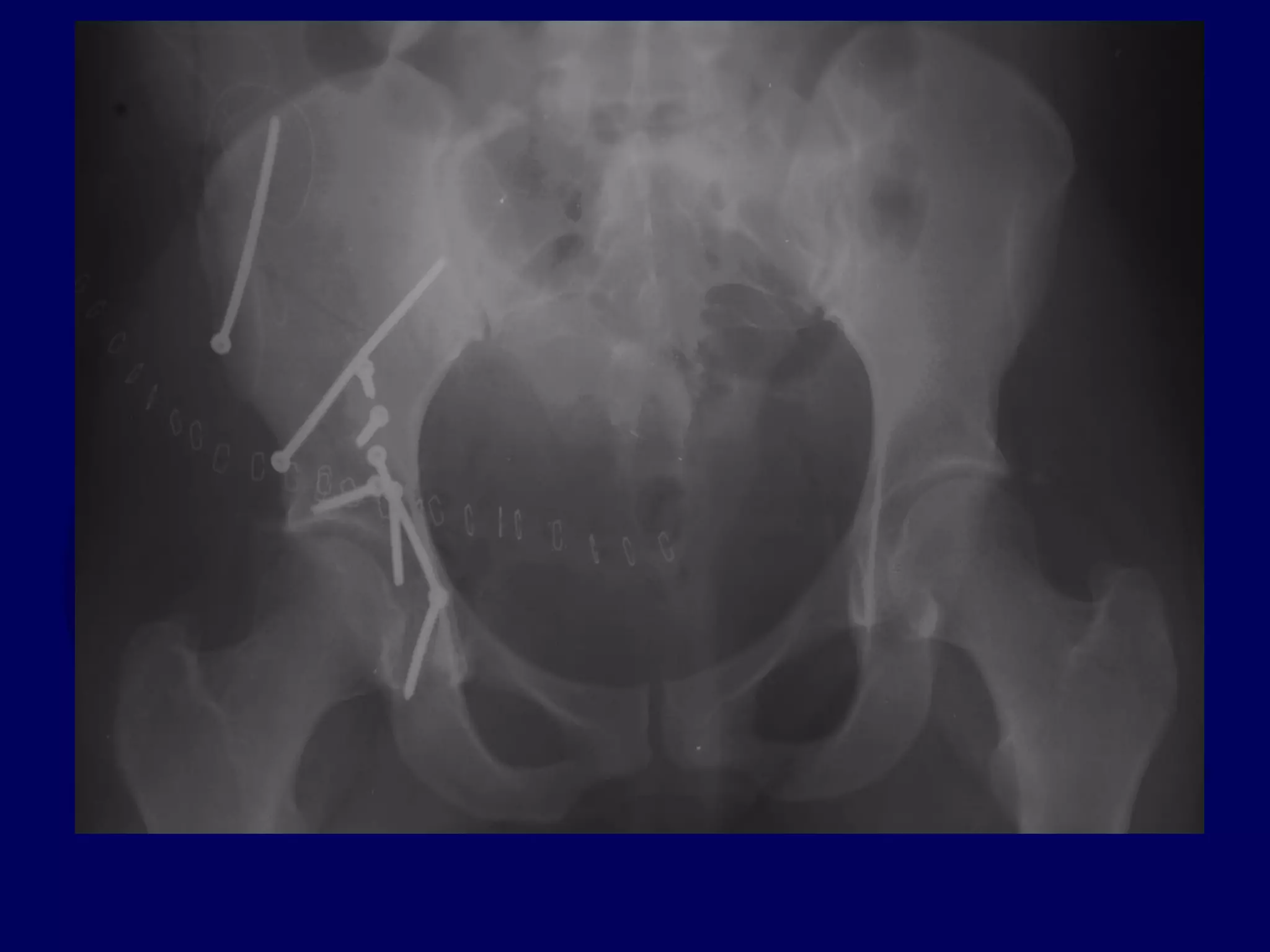
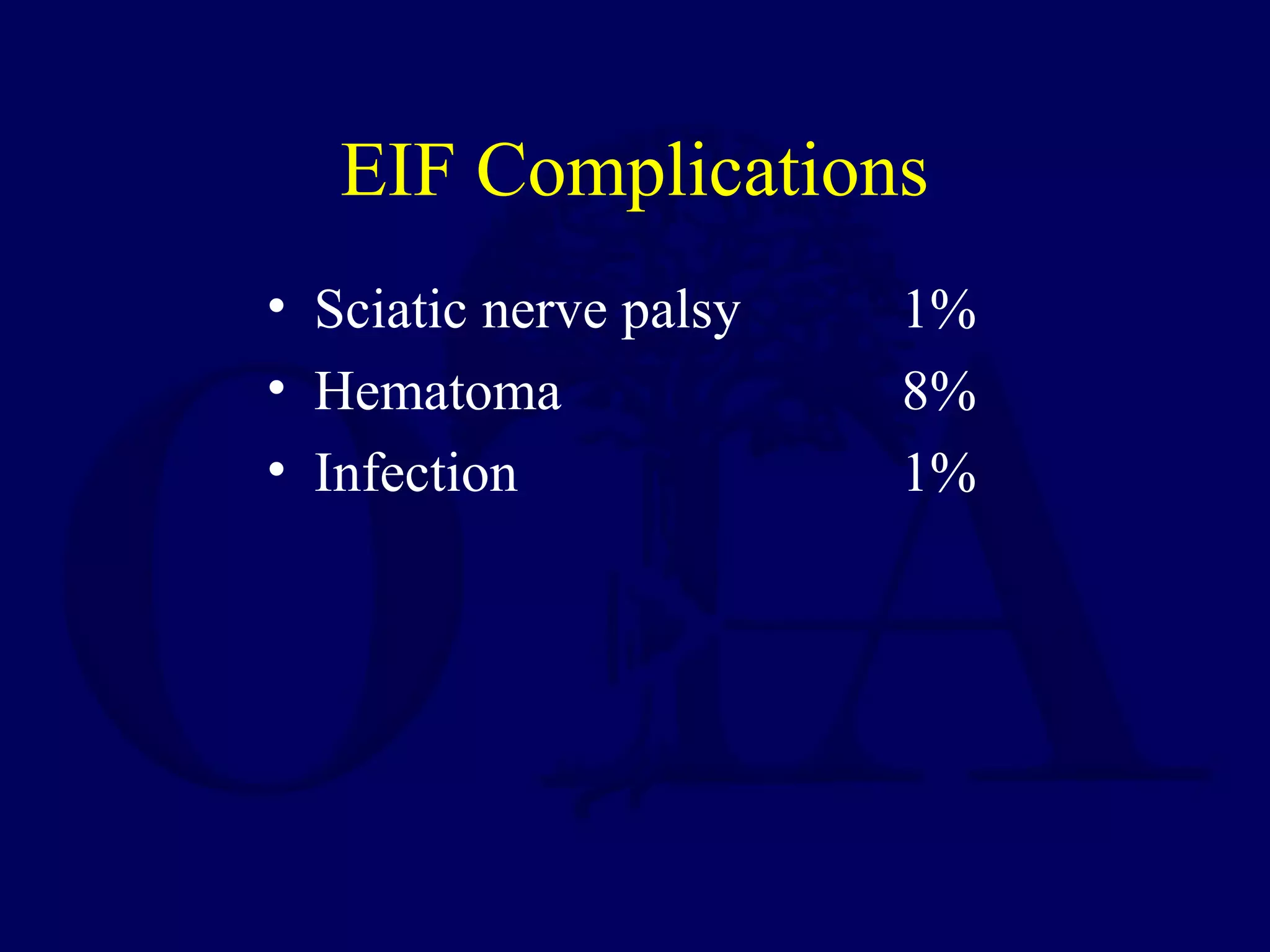
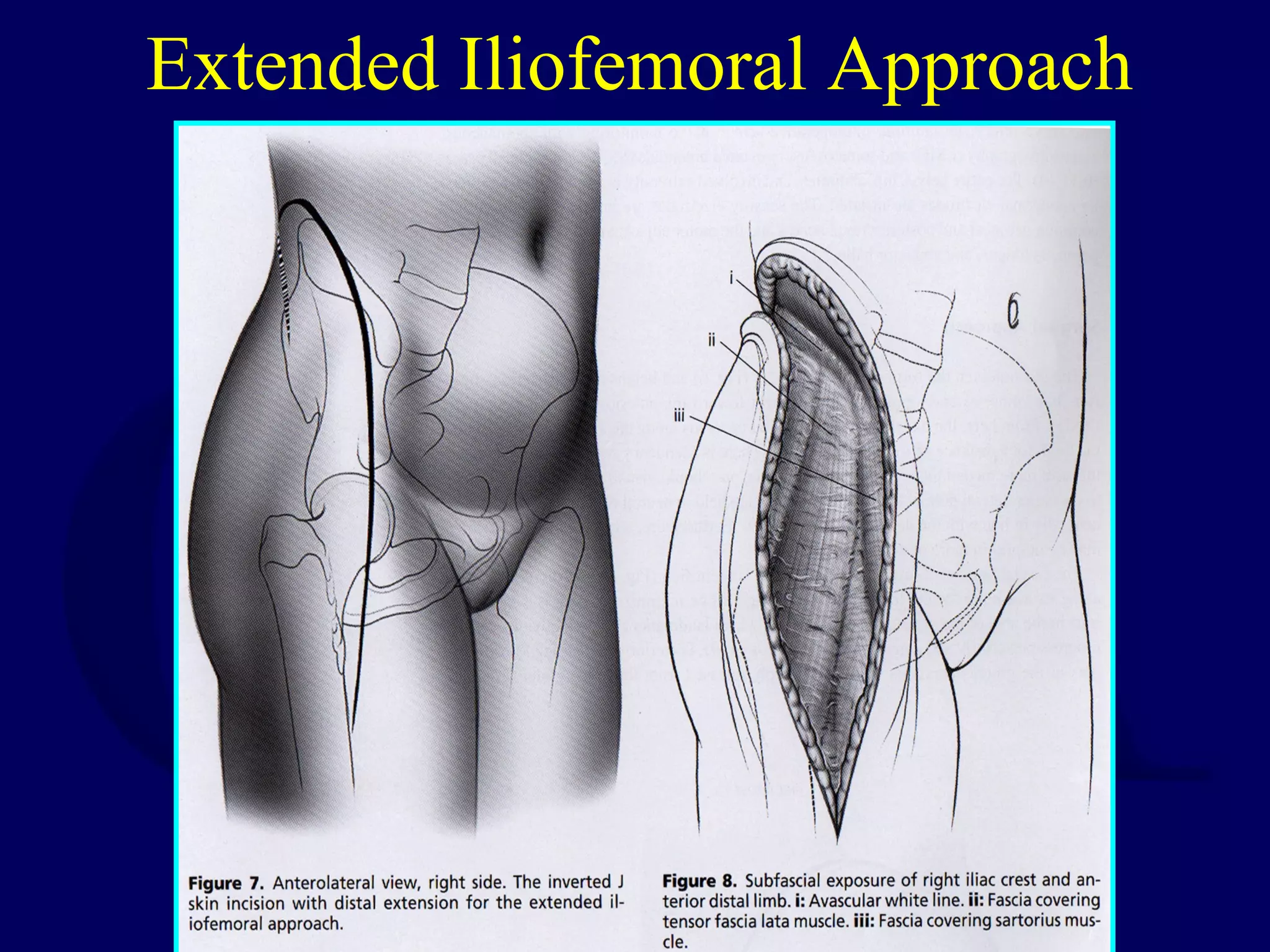
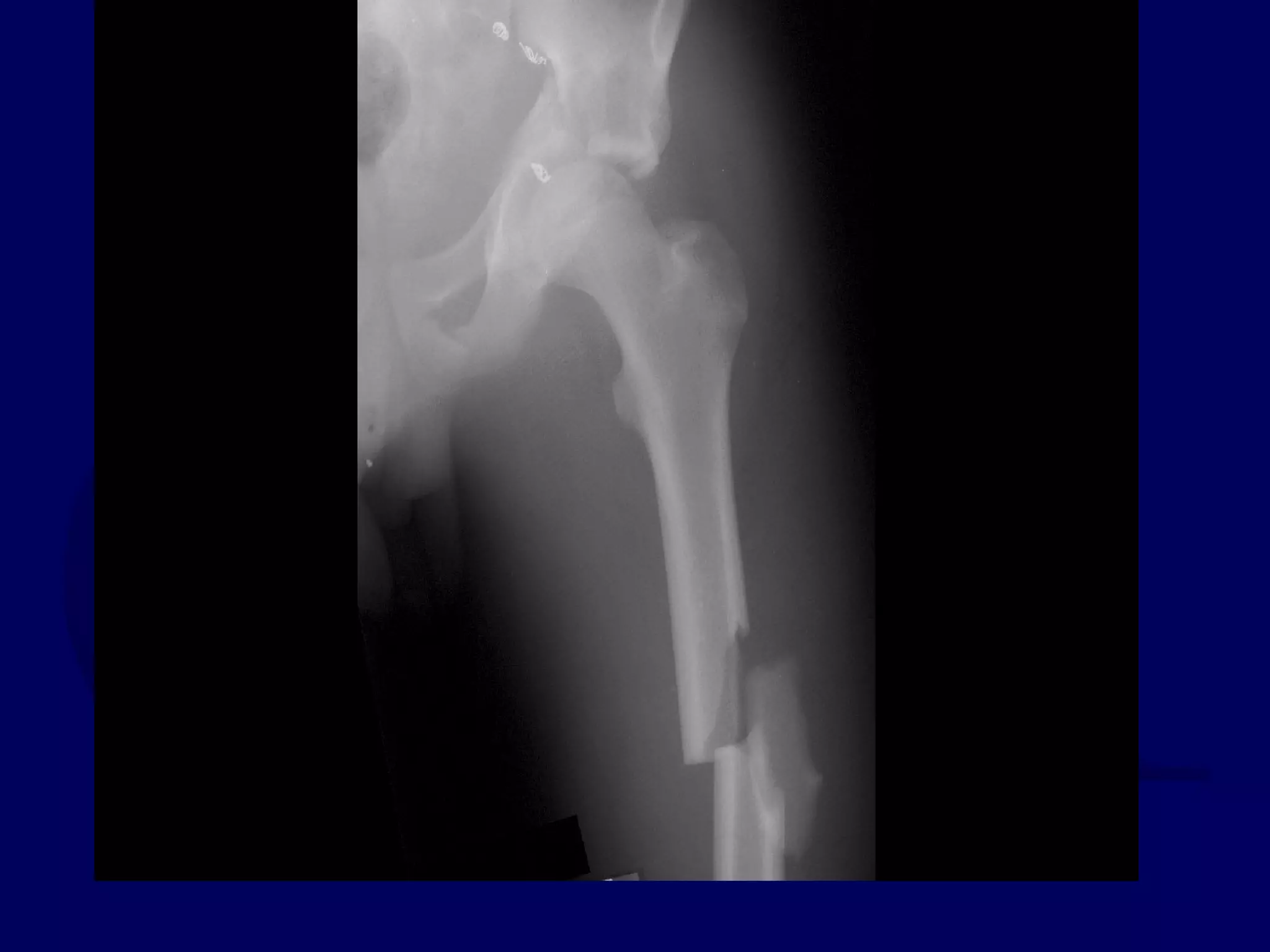
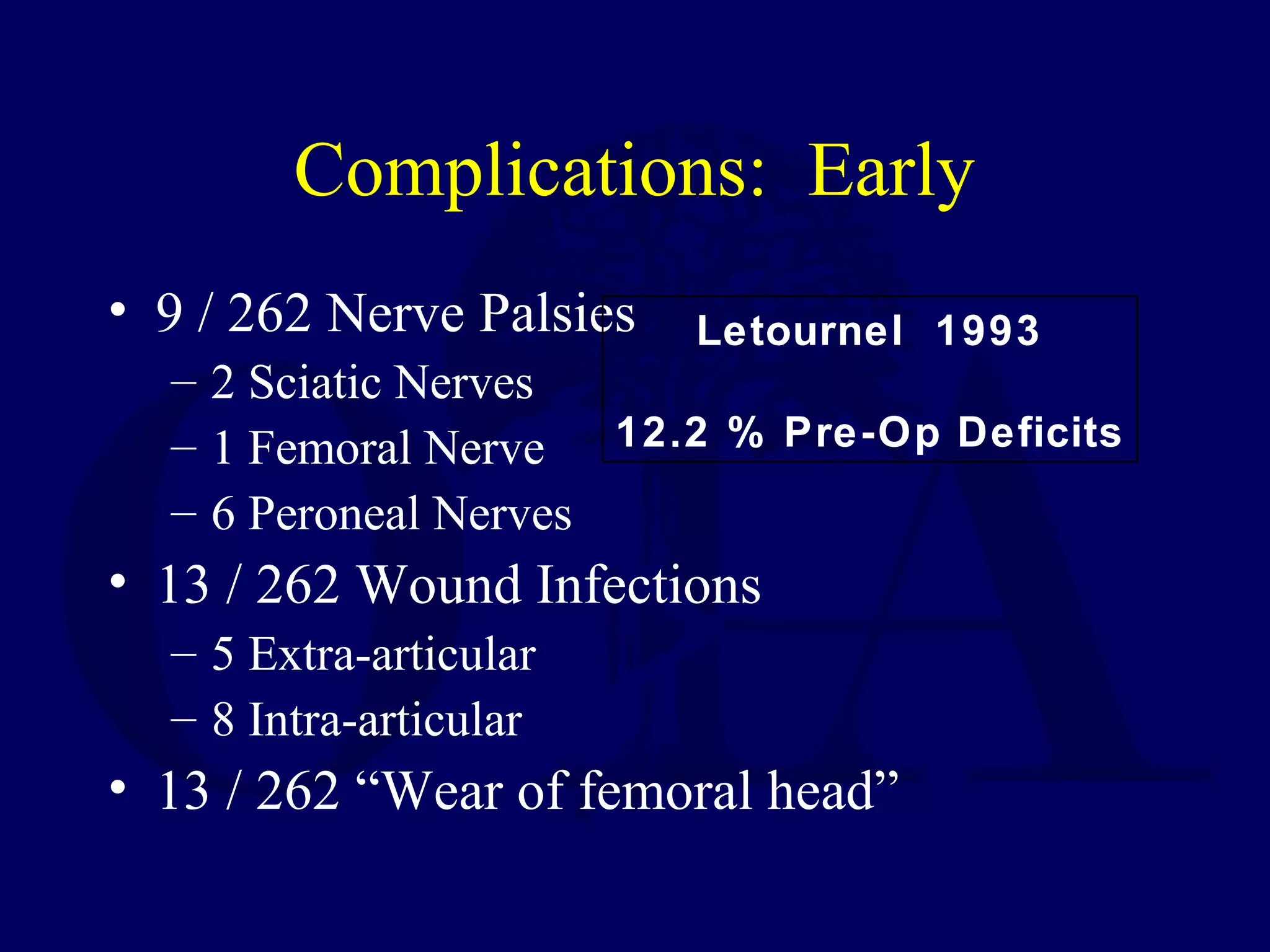
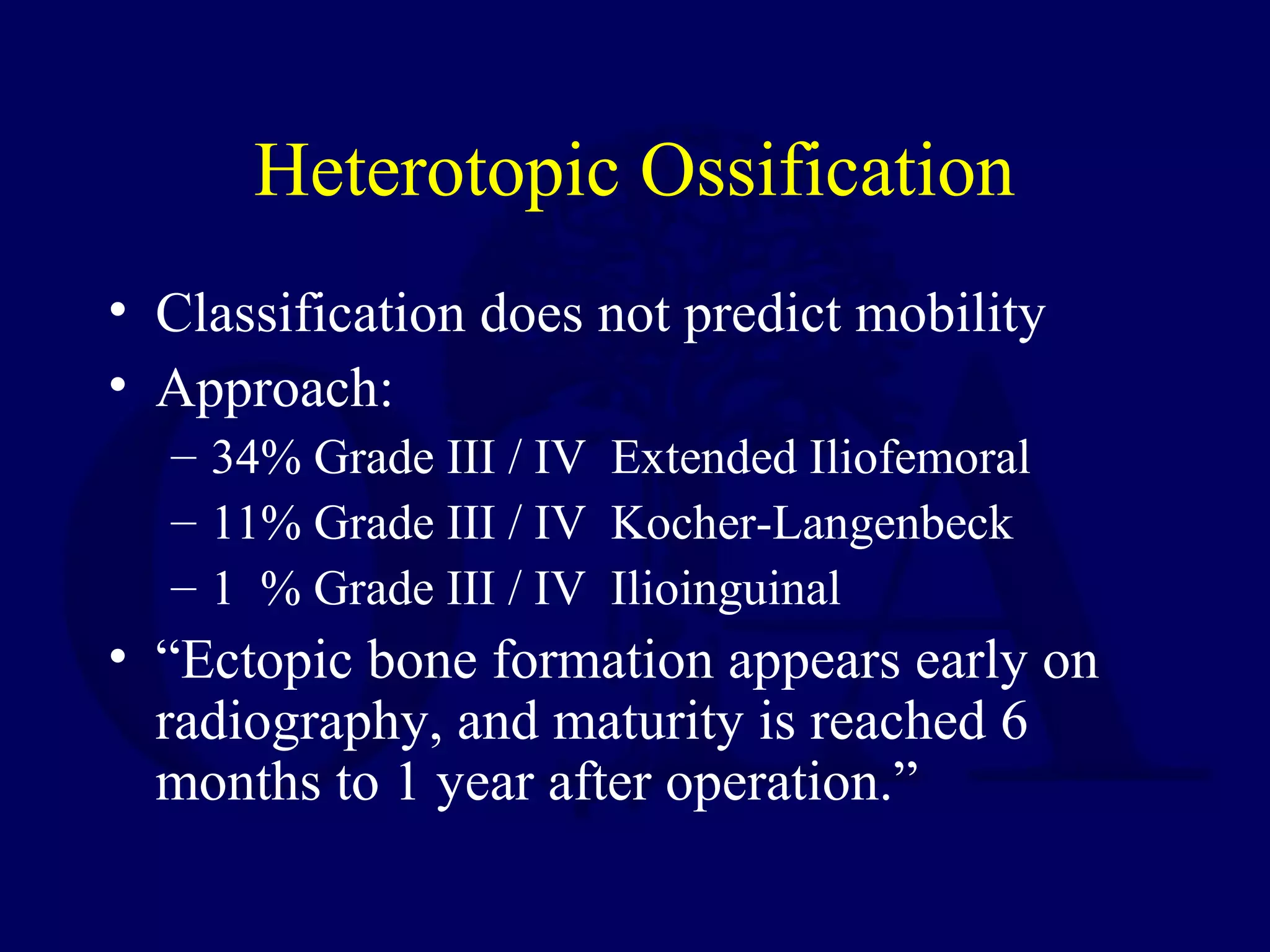
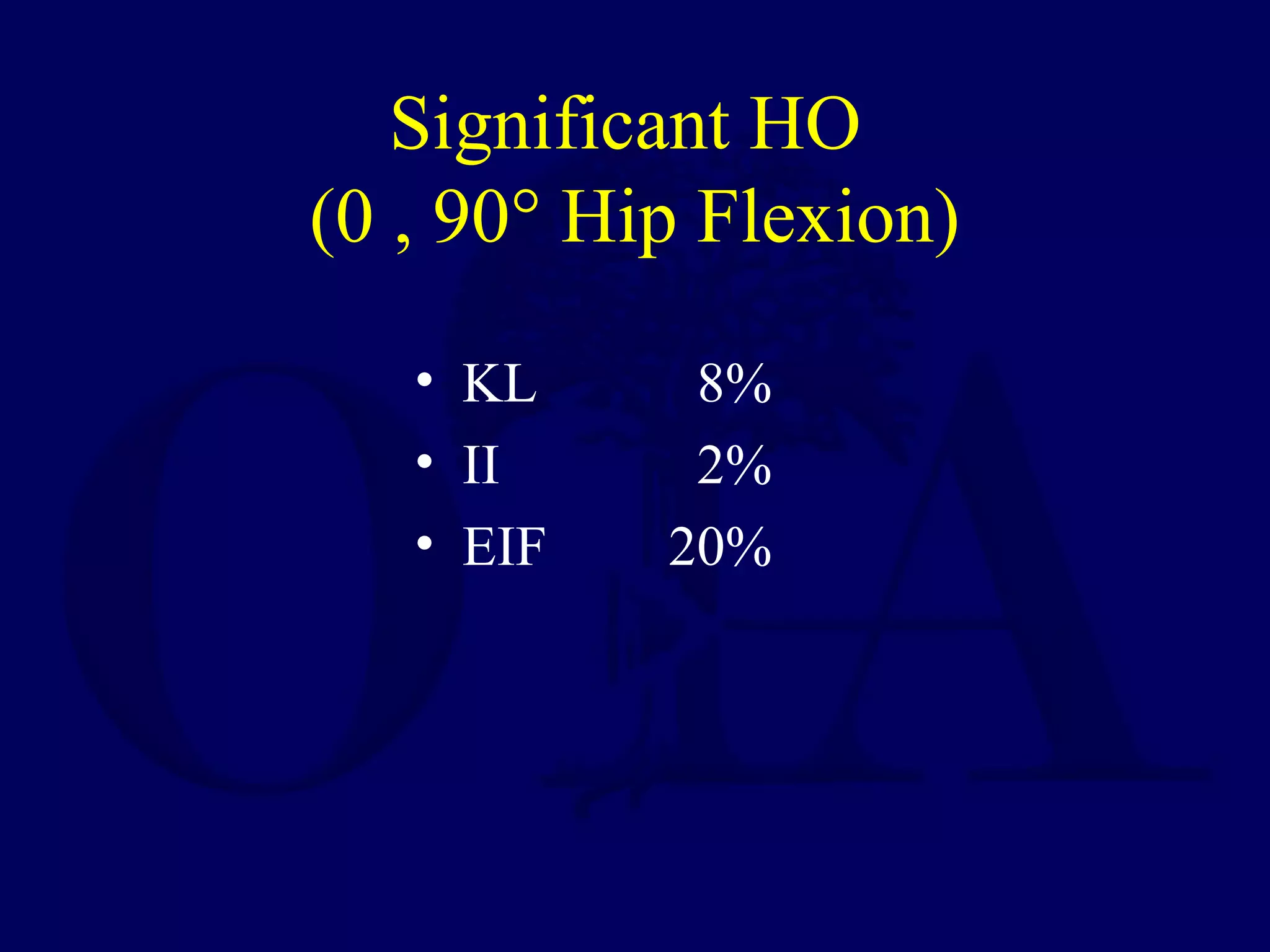
This document summarizes surgical management of acetabular fractures. It discusses the goals of operative management as anatomic reduction and different surgical approaches for specific fracture patterns. The Kocher-Langenbeck approach is indicated for posterior wall, column and transverse fractures involving the posterior region. The ilioinguinal approach is used for anterior wall, column and transverse fractures involving the anterior region. Perfect anatomic reduction is important for excellent outcomes, and timing of surgery within 2 weeks can improve chances of anatomic reduction. Complications of each approach are discussed.