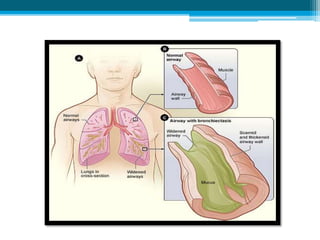
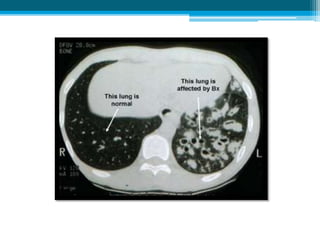
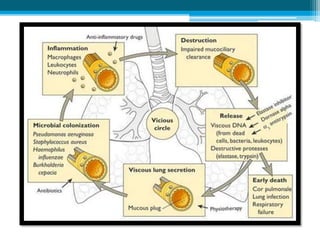
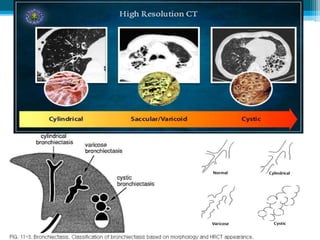
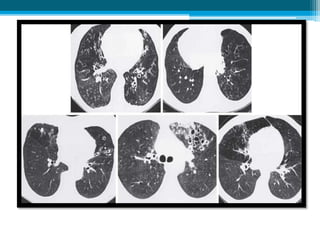
Bronchiectasis is a chronic condition characterized by the permanent dilation and destruction of bronchi, primarily due to difficulty in clearing secretions and recurrent infections. It can be congenital or acquired, with various associated diseases, and presents symptoms such as chronic productive cough and copious purulent sputum. Diagnosis involves thin-section HRCT scans, while treatment focuses on reducing airway obstruction and controlling infections, often requiring antibiotics and airway hydration.