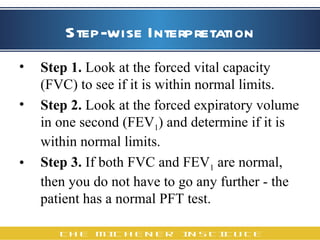
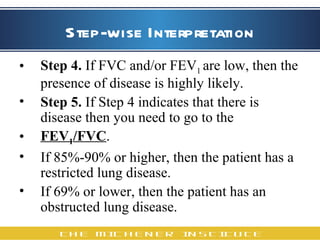
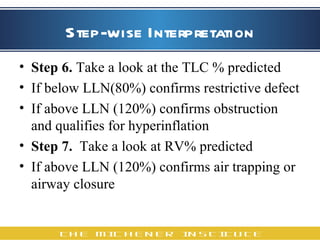
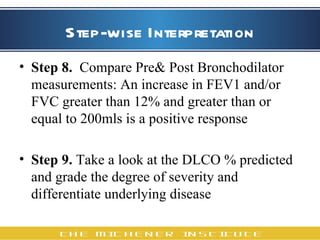
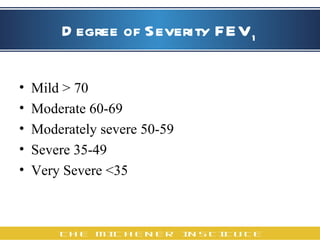
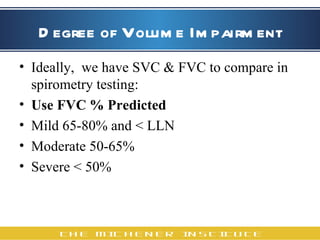
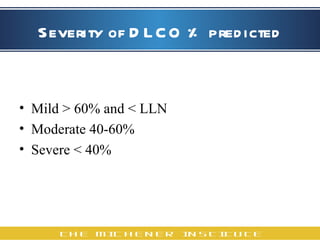
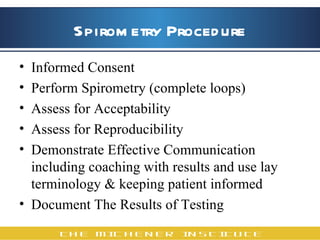
The document outlines the step-by-step process for interpreting spirometry tests according to American Thoracic Society (ATS) guidelines. It discusses evaluating forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FEV1/FVC ratio, total lung capacity (TLC), residual volume (RV), and diffusing capacity of the lung for carbon monoxide (DLCO) to determine if values are normal or indicate restrictive or obstructive lung disease. Severity is classified based on percentage of predicted values. The document also reviews procedures for informed consent, performing acceptable and reproducible spirometry tests, and documenting and communicating results.