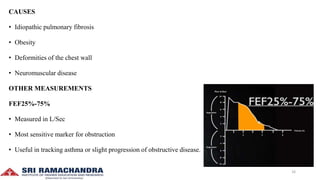
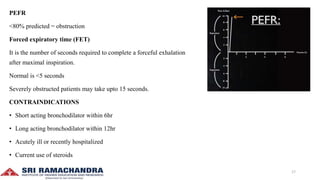
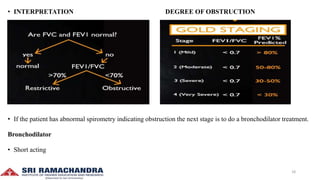
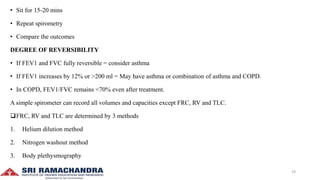
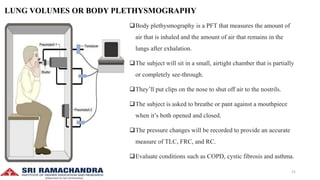
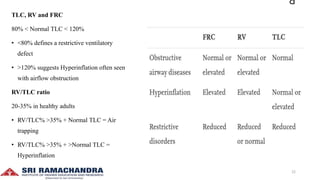
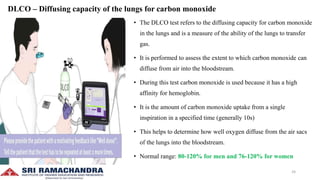
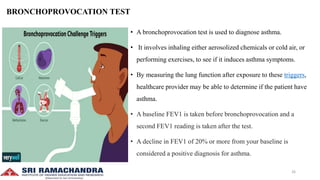
Pulmonary function tests (PFTs) are critical evaluations used to assess respiratory health by measuring lung volume, capacity, flow rate, and gas exchange, aiding in diagnosing obstructive and restrictive lung diseases. Tests like spirometry and diffusing capacity for carbon monoxide (DLCO) help determine the severity of conditions such as asthma, COPD, and pulmonary fibrosis. The document outlines various lung volumes, capacities, and specific tests, detailing their procedures and interpretation in clinical practice.