The document discusses blood, tissue fluid, and lymph. It describes:
1) Blood plasma as a pale yellow liquid consisting mainly of water with dissolved substances and no blood cells.
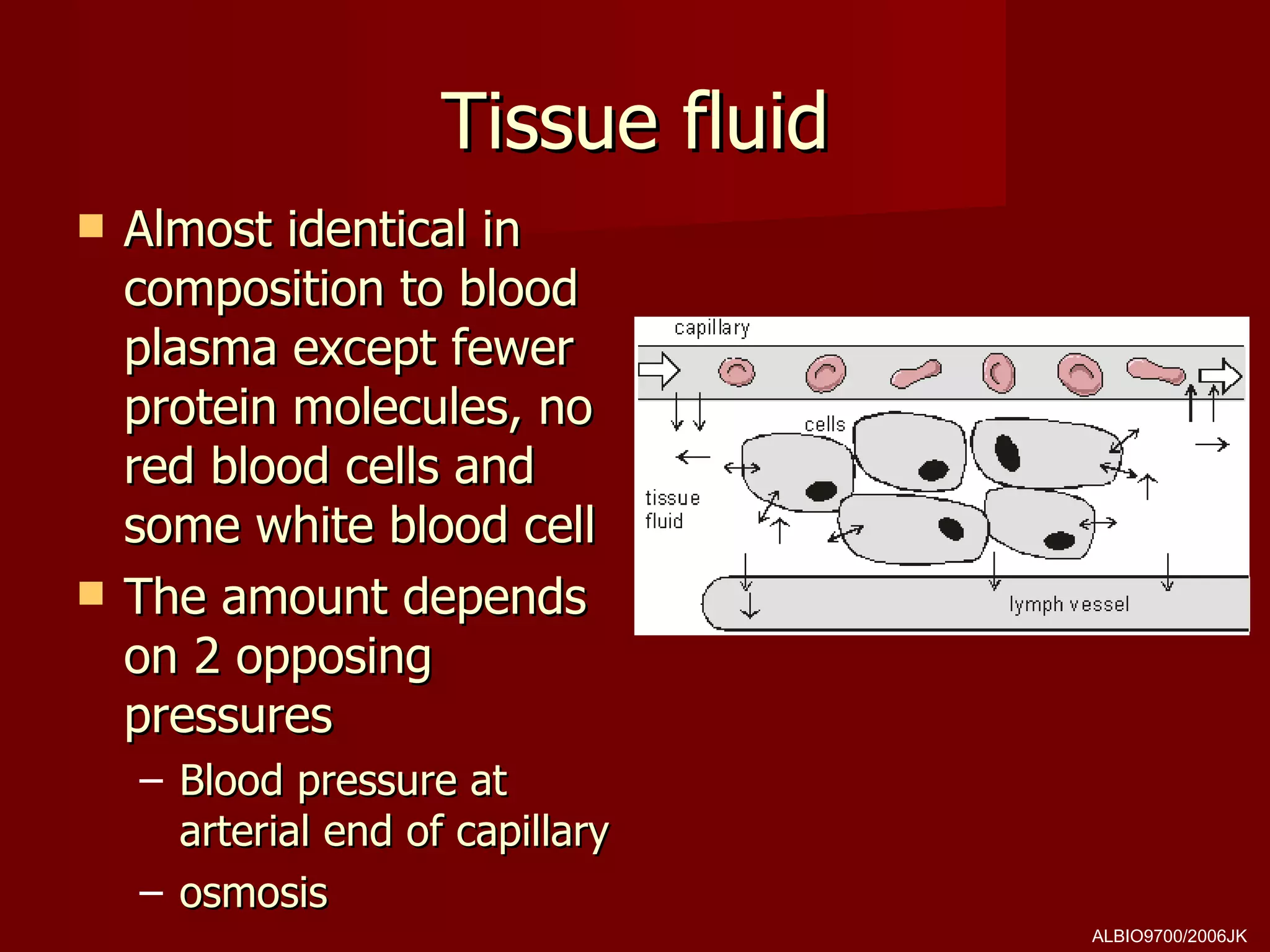
2) Tissue fluid as similar in composition to blood plasma but with fewer proteins, no blood cells, and varying amounts depending on pressures between blood vessels and tissues.
3) Lymph as collected tissue fluid that is returned to blood vessels through lymphatic vessels, maintaining tissue fluid composition.