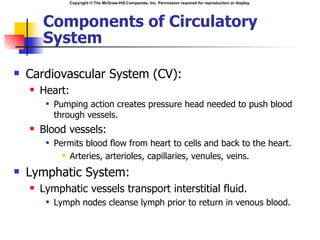
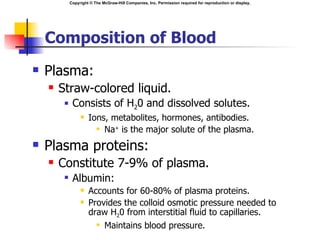
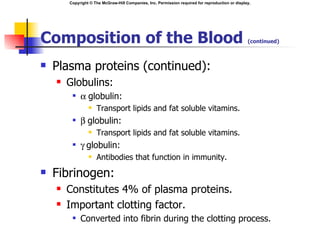
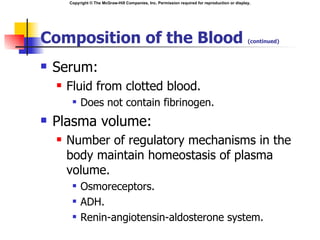
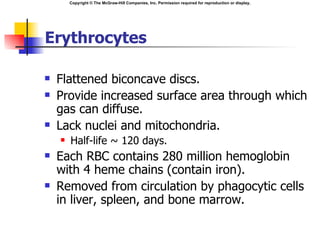
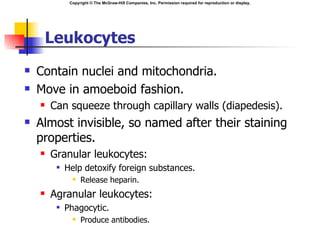
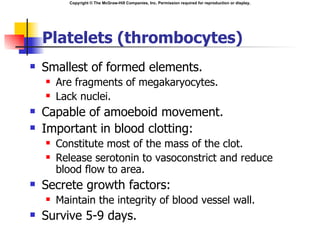
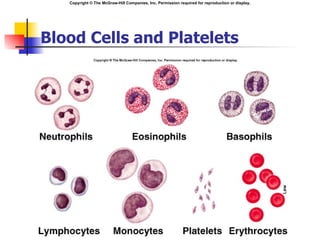
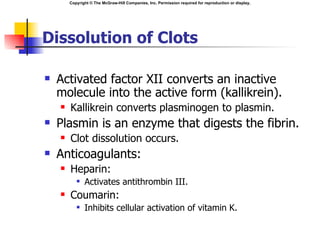
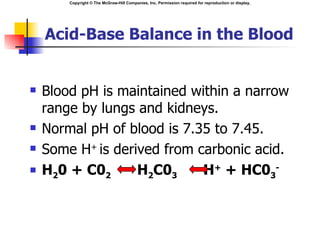
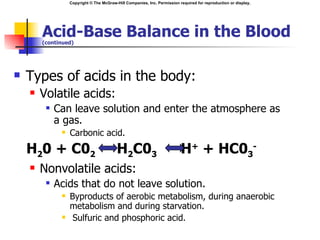
The document describes the circulatory system and its functions. It discusses the components of blood including plasma, erythrocytes, leukocytes, and platelets. It explains hematopoiesis, blood typing, clotting, and acid-base balance. Key points include that the circulatory system transports nutrients, gases, hormones, and wastes. It regulates temperature and protects against pathogens. Blood is composed of plasma, blood cells, and platelets which are produced through hematopoiesis in the bone marrow.
![Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
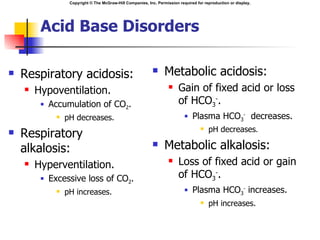
pH
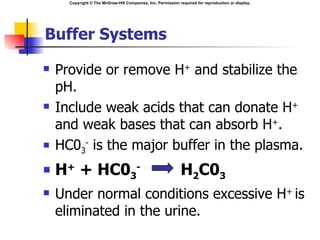
Normal pH is obtained when the ratio of
HCO3- to C02 is 20:1.
Henderson-Hasselbalch equation:
pH = 6.1 + log = [HCO3-]
[0.03PC02]](https://image.slidesharecdn.com/heartcirculation-120511091224-phpapp01/85/Heart-circulation-29-320.jpg)
![Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
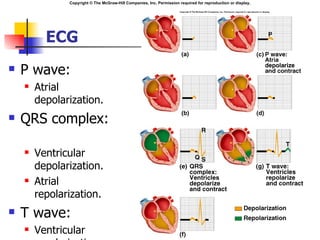
Electrocardiogram (ECG/EKG)
The body is a good conductor of electricity.
Tissue fluids have a high [ions] that move in
response to potential differences.
Electrocardiogram:
Measure of the electrical activity of the heart
per unit time.
Potential differences generated by heart are conducted
to body surface where they can be recorded on
electrodes on the skin.
Does NOT measure the flow of blood through
the heart.](https://image.slidesharecdn.com/heartcirculation-120511091224-phpapp01/85/Heart-circulation-49-320.jpg)
![Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Ischemic Heart Disease
Ischemia:
Oxygen supply to tissue
is deficient.
Most common cause is
atherosclerosis of
coronary arteries.
Increased [lactic acid]
produced by anaerobic
respiration.
Angina pectoris:
Substernal pain.
Myocardial infarction
(MI):
Changes in T segment of
ECG.
Increased CPK and LDH.](https://image.slidesharecdn.com/heartcirculation-120511091224-phpapp01/85/Heart-circulation-62-320.jpg)