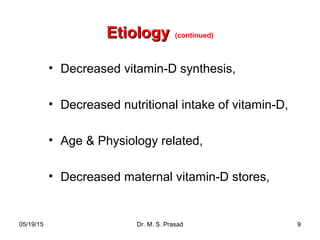
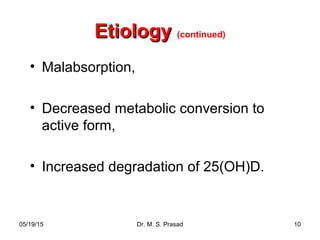
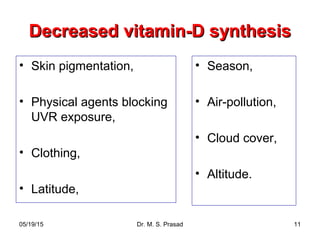
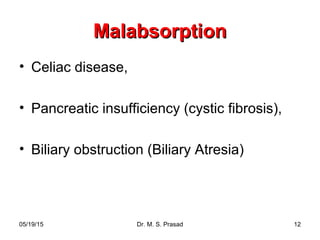
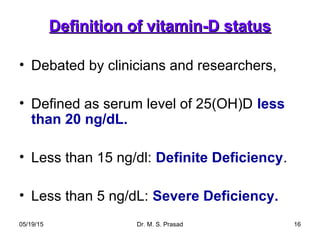
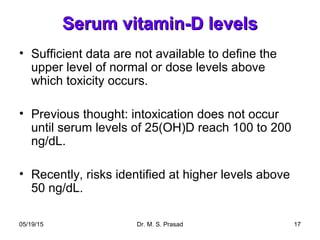
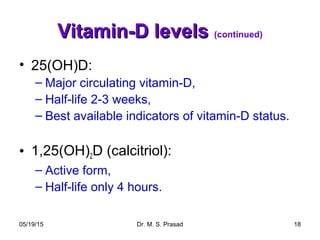
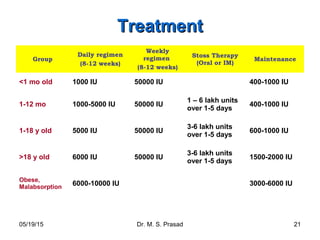
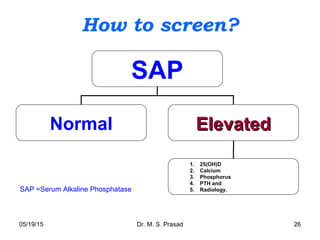
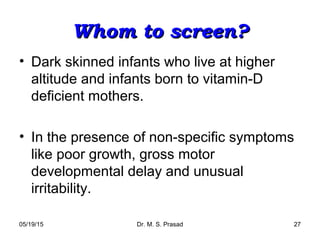
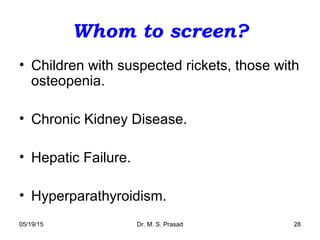
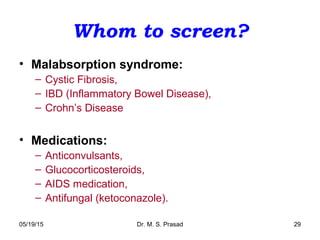
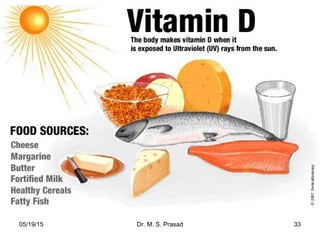
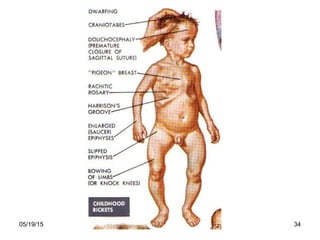
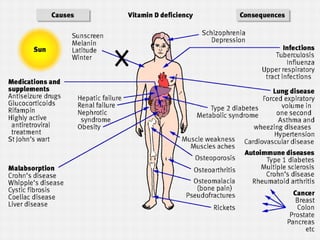
Vitamin D deficiency is a widespread problem globally and in India. It can cause rickets in children and bone problems in adults. The document discusses the causes, presentation, diagnosis, and treatment of vitamin D deficiency. Key points include that it is caused by low dietary intake and sun exposure, symptoms range from bone pain to rickets, screening involves vitamin D and calcium levels as well as imaging, and treatment consists of high dose vitamin D supplements and calcium for several weeks.