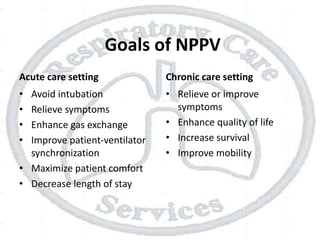
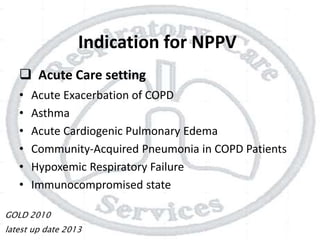
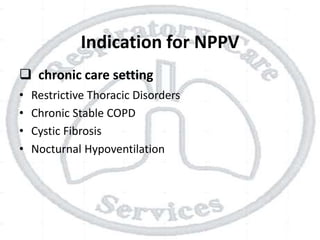
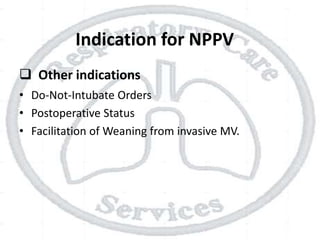
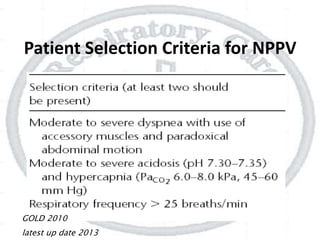
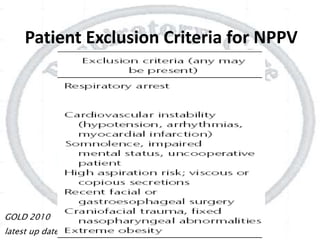
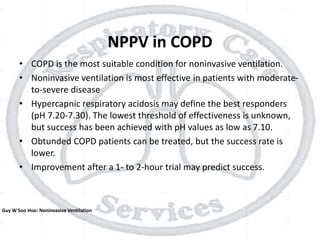
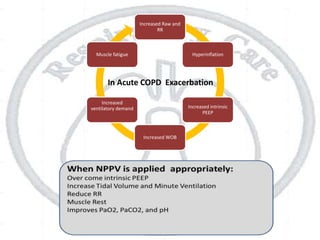
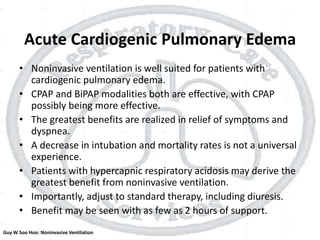
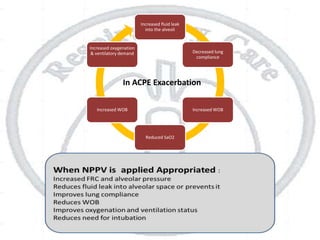
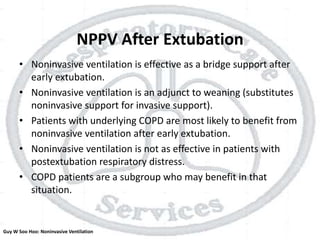
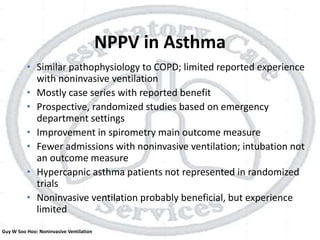
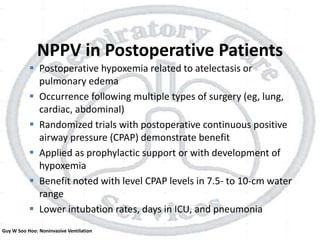
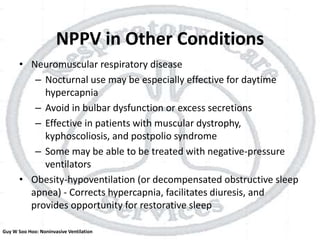
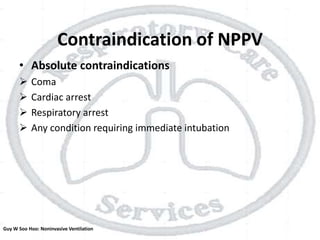
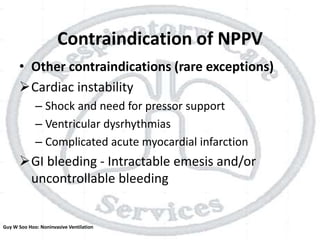
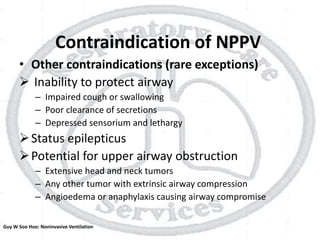
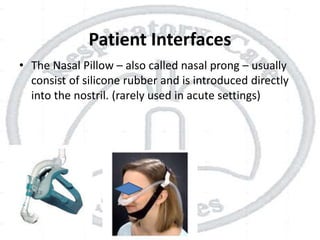
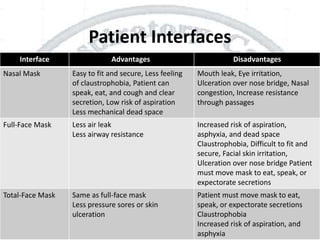
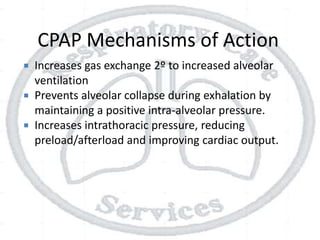
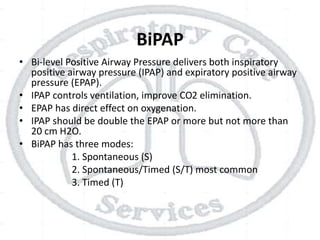
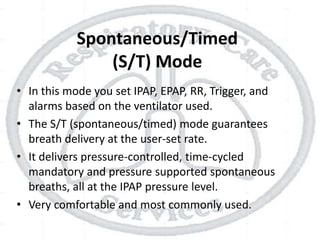
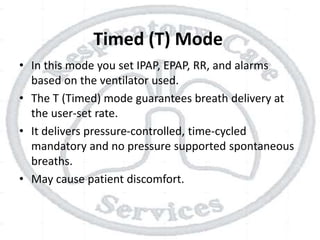
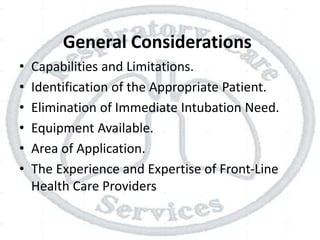
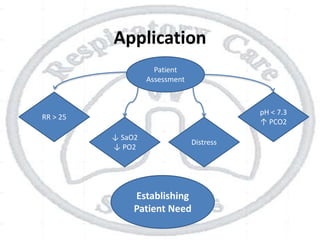
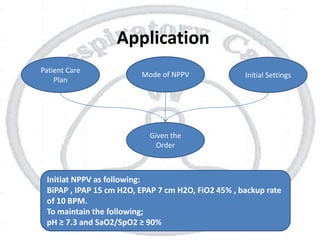
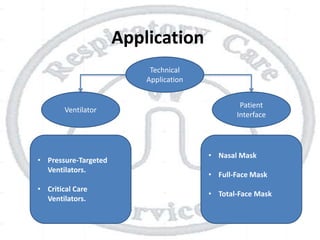
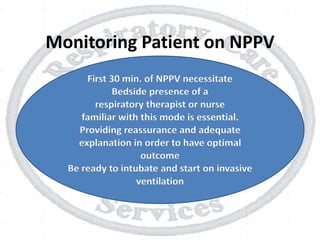
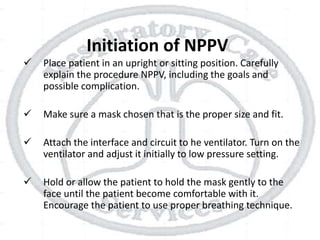
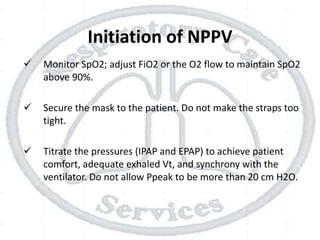
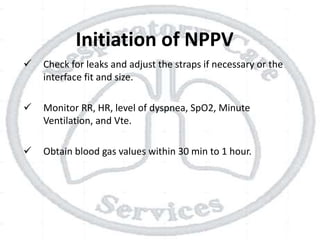
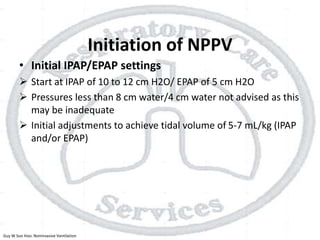
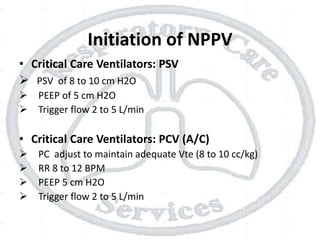
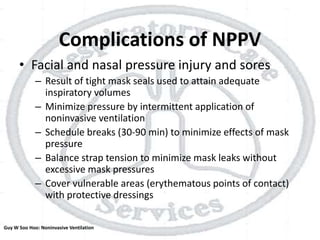
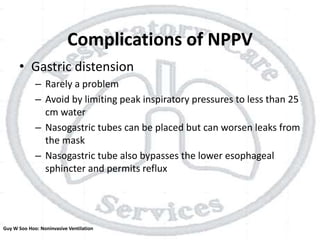
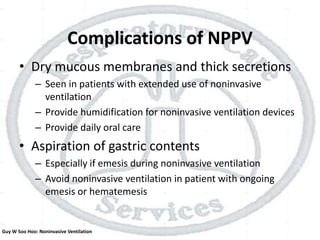
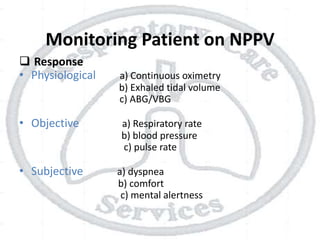
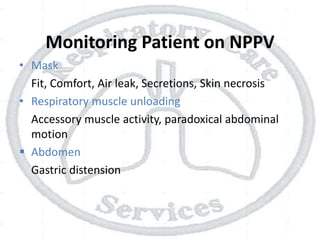
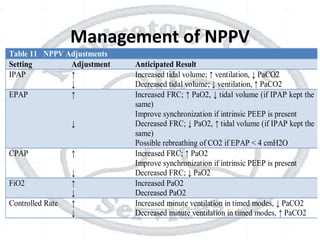
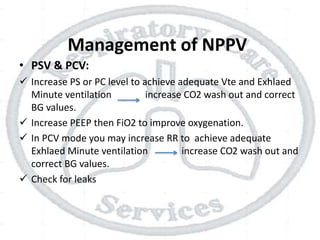
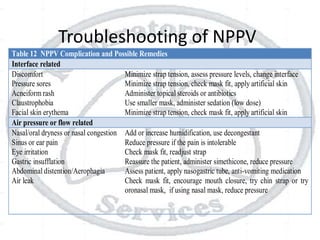
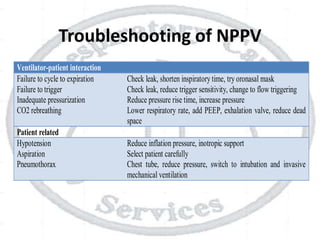
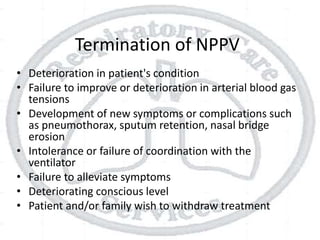
The document outlines non-invasive positive pressure ventilation (NPPV), including its definition, goals, indications, patient selection criteria, contraindications, equipment, modes of ventilation, how to initiate NPPV, complications, monitoring, and troubleshooting. NPPV can be used to treat acute exacerbations of COPD, asthma, acute cardiogenic pulmonary edema, and other conditions. The goals of NPPV are to avoid intubation, relieve symptoms, enhance gas exchange, and improve patient comfort.