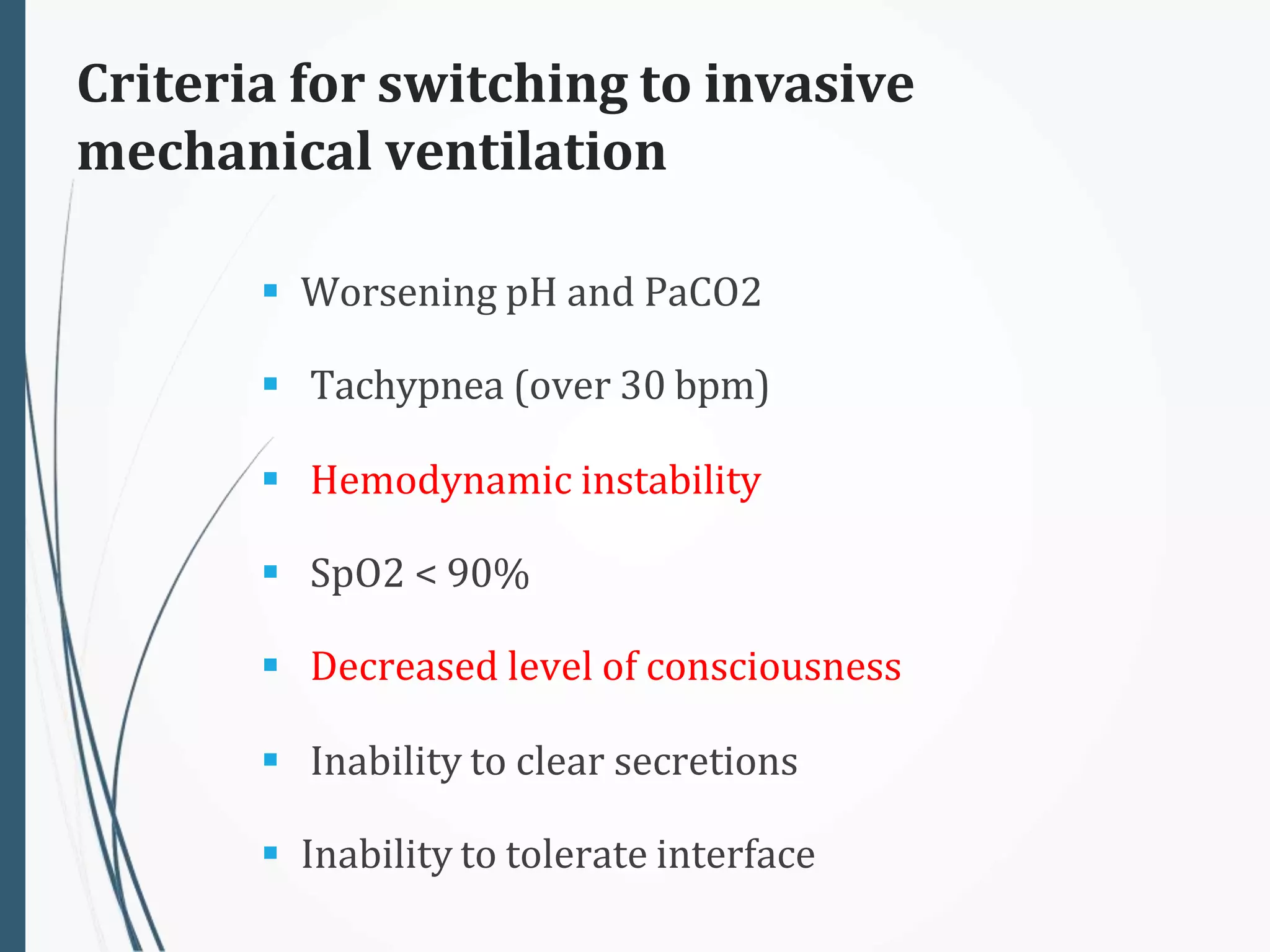
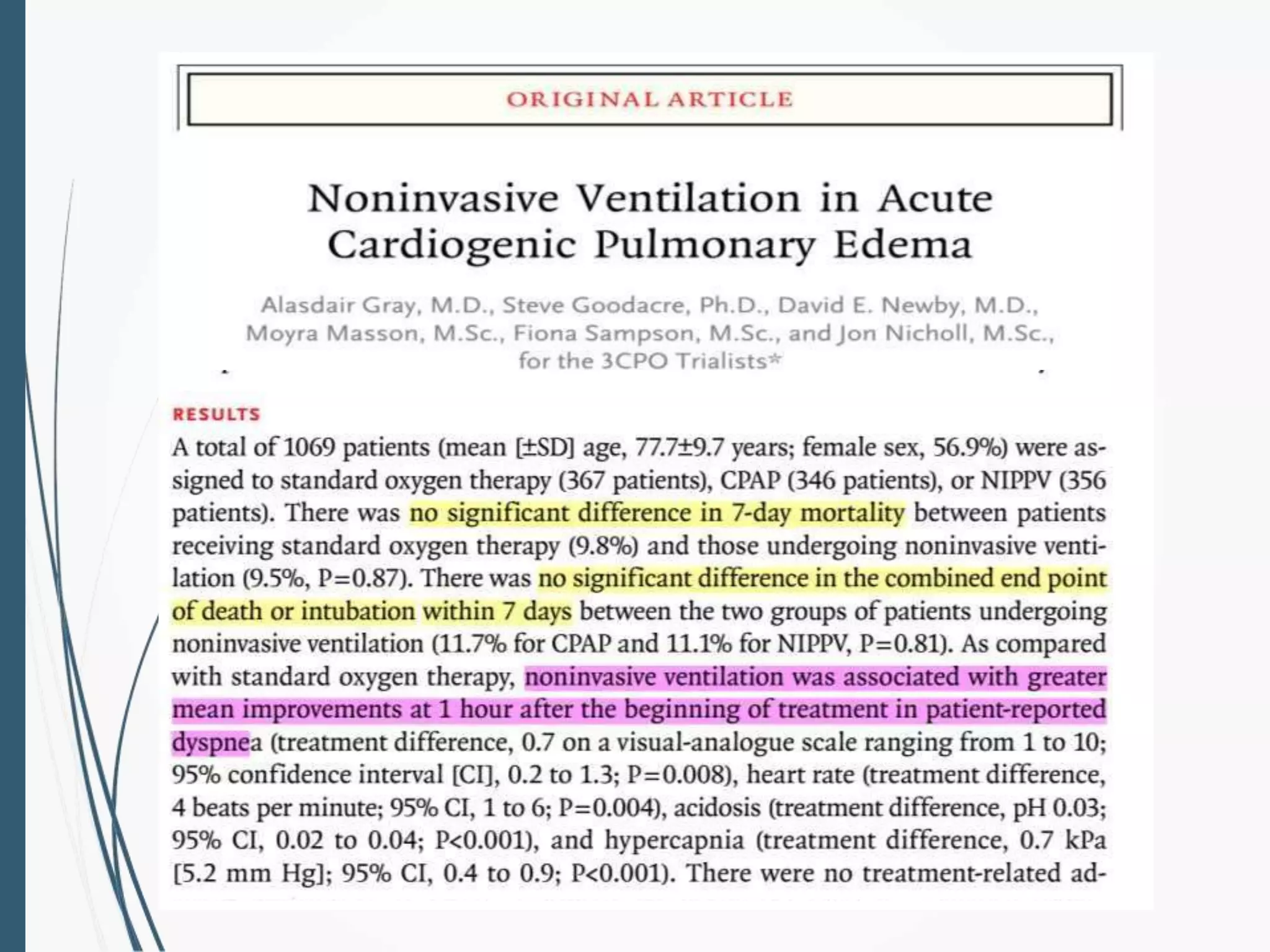
Non-invasive ventilation (NIV) was initially developed to treat polio victims and patients with obstructive sleep apnea. It involves delivering ventilation without intubation by using interfaces like nasal or facial masks connected to ventilators. NIV can be delivered via several modes and is used to treat conditions like COPD exacerbations, cardiogenic pulmonary edema, immunocompromised patients with pneumonia, and as a bridge to weaning from mechanical ventilation or for palliative care. Close monitoring is required as NIV may fail and require intubation. Guidelines provide conditional or strong recommendations for its use in specific acute and chronic clinical situations.