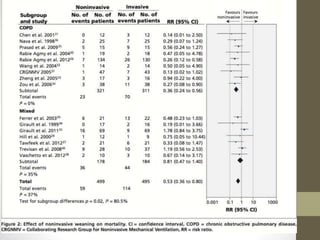
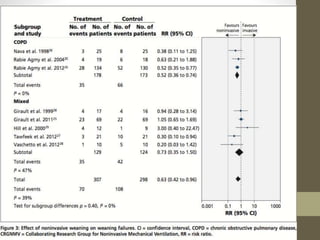
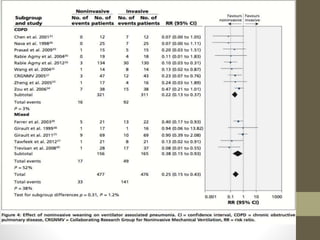
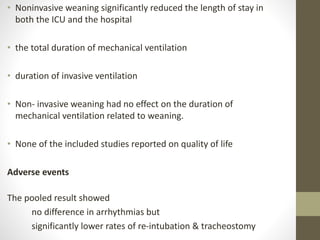
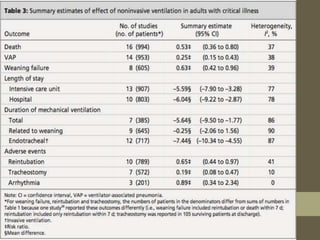
Noninvasive ventilation may provide benefits as a weaning strategy compared to invasive weaning from mechanical ventilation. A systematic review and meta-analysis of randomized controlled trials found that noninvasive weaning significantly reduced mortality, rates of weaning failure and ventilator-associated pneumonia. It also decreased length of stay in the ICU and hospital as well as total duration of mechanical ventilation compared to invasive weaning. Subgroup analysis showed greater reduction in mortality for patients with COPD using noninvasive weaning.