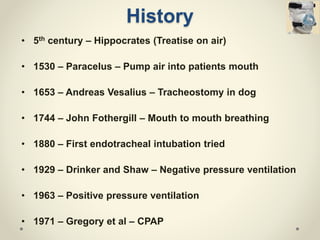
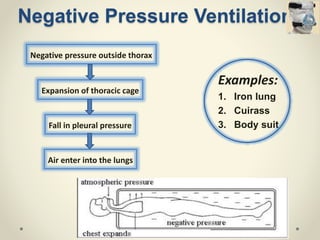
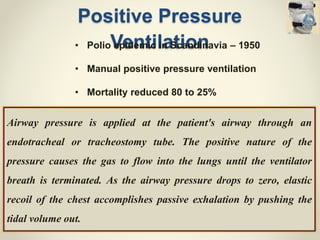
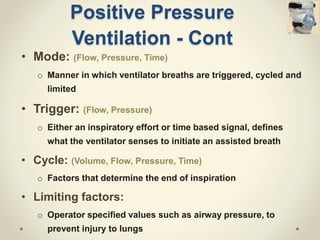
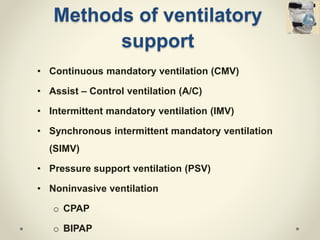
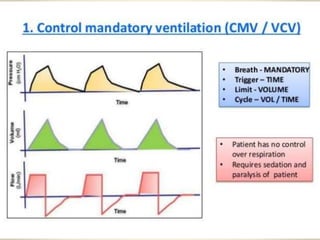
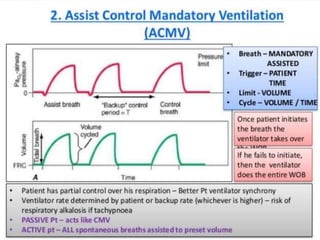
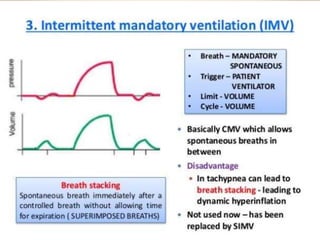
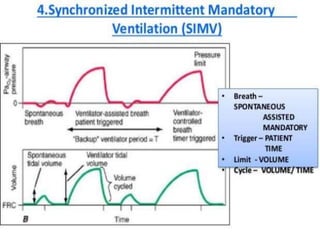
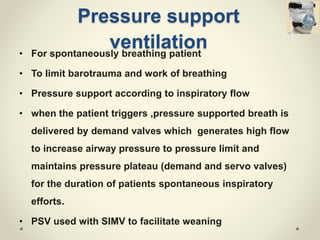
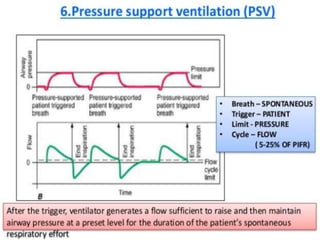
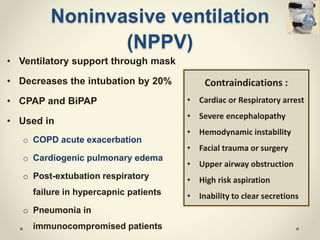
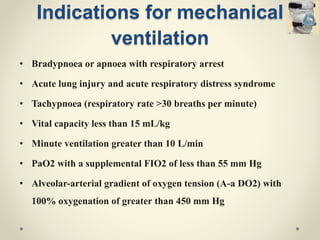
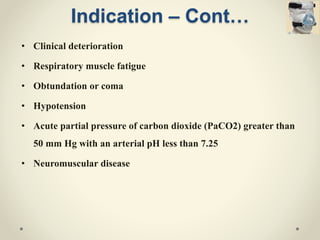
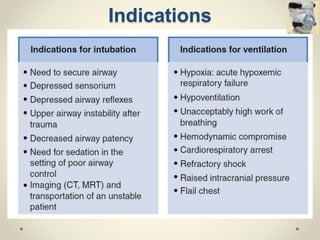
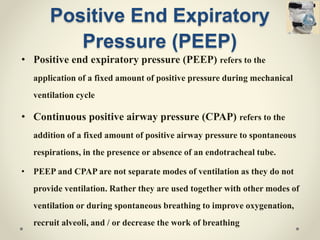
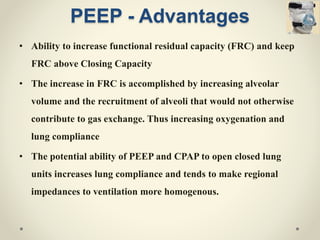
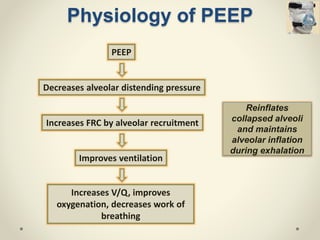
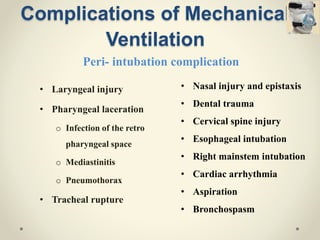
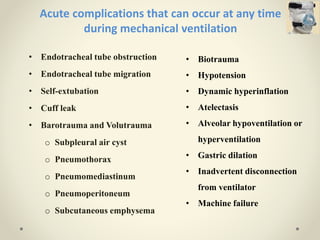
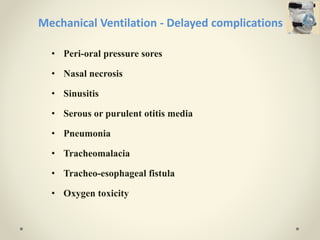
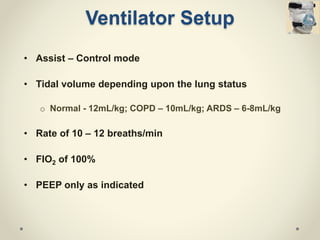
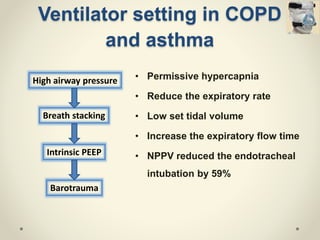
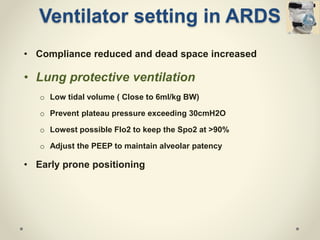
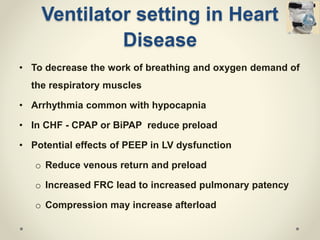
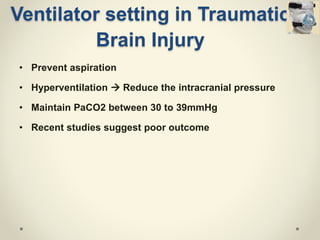
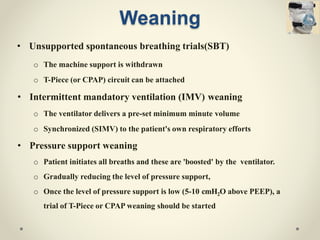
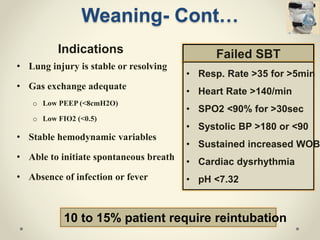
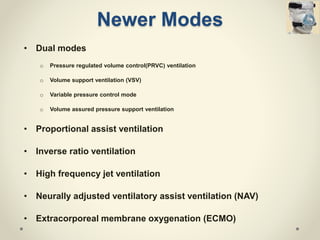
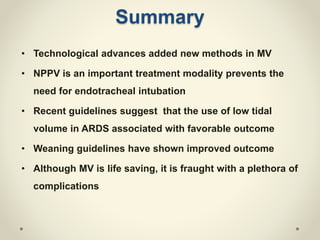
This document provides an overview of mechanical ventilation including its history, types of ventilators, modes of ventilation, indications, complications, ventilator settings for specific diseases, weaning methods, and newer methods. It discusses positive pressure ventilation and various modes like CMV, A/C, IMV, SIMV, and PSV. Complications of mechanical ventilation include barotrauma, volutrauma, VAP, and oxygen toxicity. Optimizing ventilator settings can reduce organ failure and duration of ventilation. Non-invasive ventilation has increased and facilitates weaning. Newer modes continue to be developed to improve ventilation support.