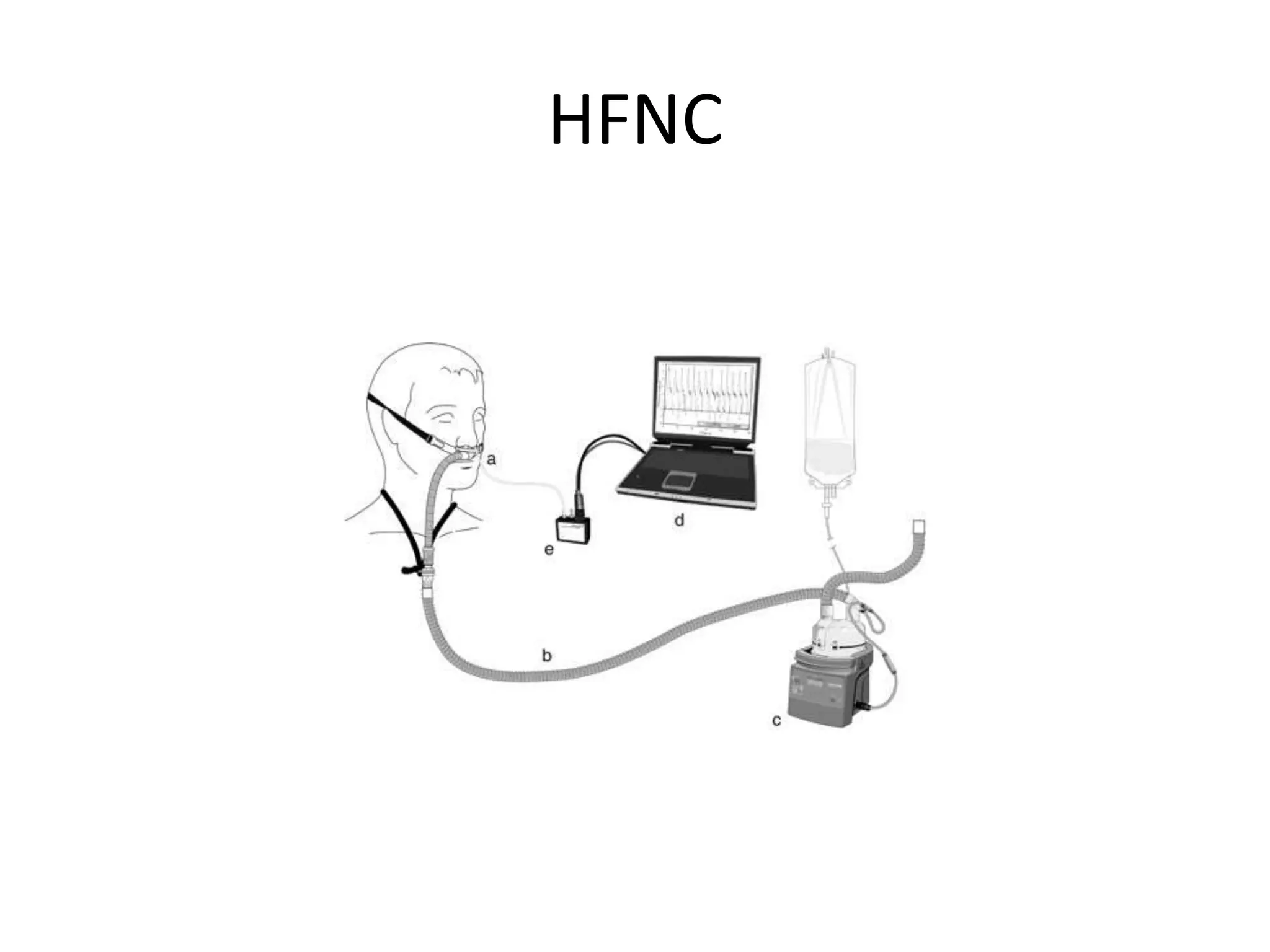
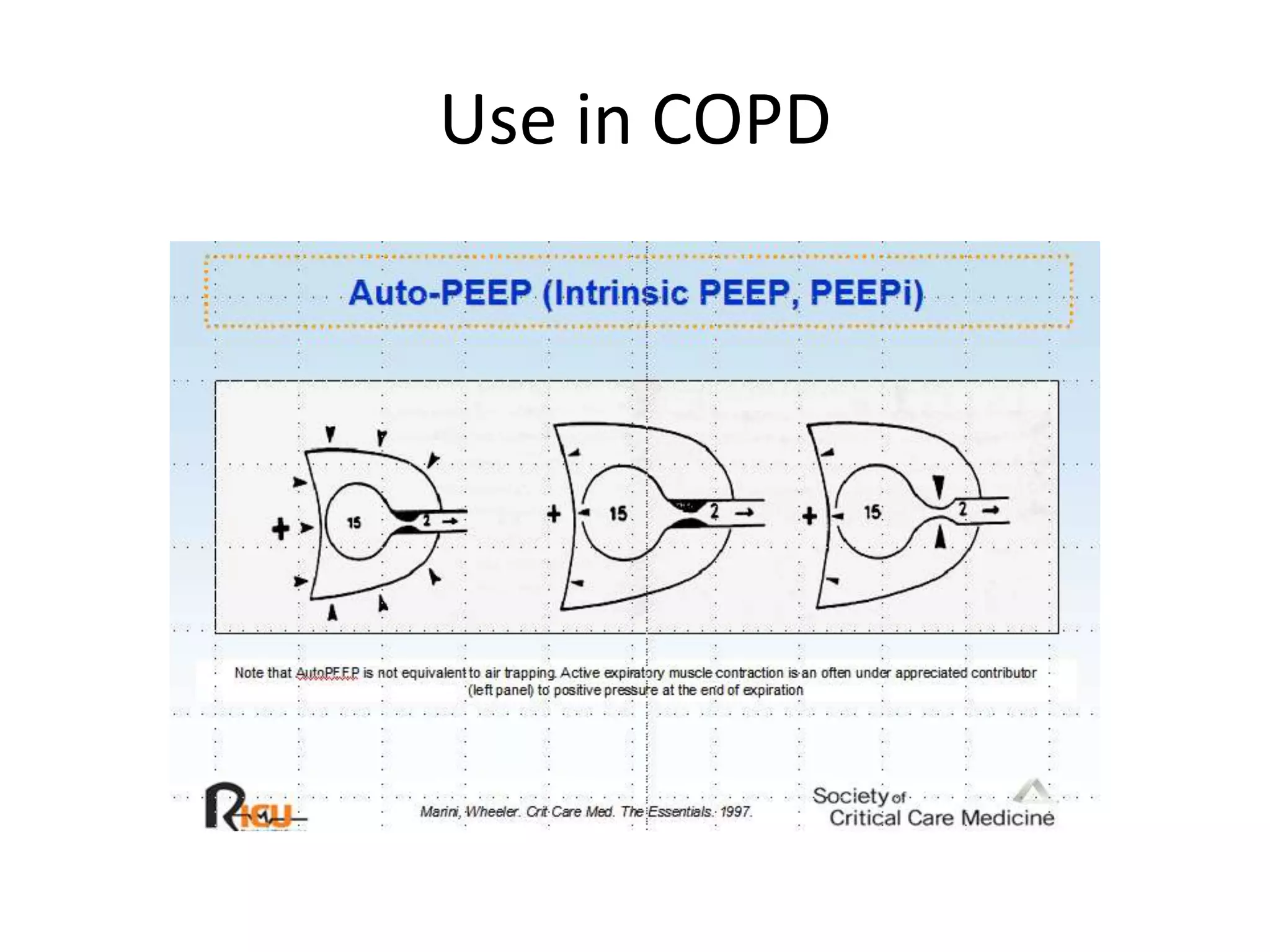
This document discusses respiratory failure and the use of high flow nasal cannula (HFNC) and bilevel positive airway pressure (BiPAP). It describes the three types of respiratory failure - inability to oxygenate, inability to ventilate, and inability to protect airway. HFNC provides high flow oxygen but no positive pressure, while BiPAP provides adjustable inspiratory and expiratory pressures for both oxygenation and ventilatory support. The document reviews indications, advantages, disadvantages, settings and monitoring for BiPAP use in treating respiratory failure.