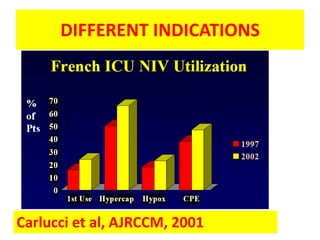
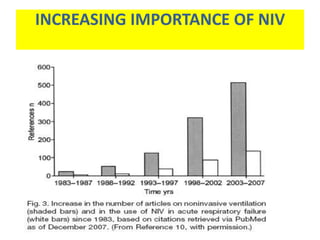
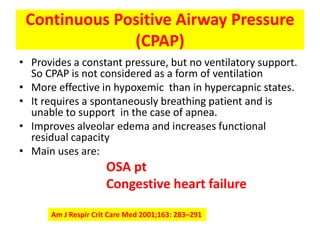
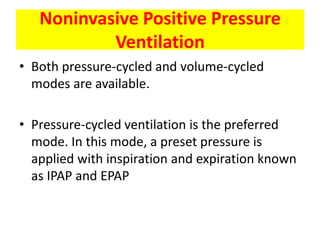
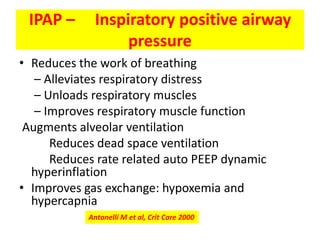
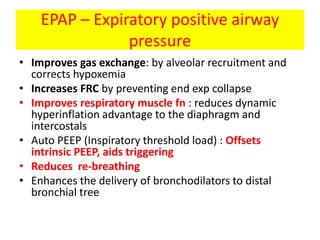
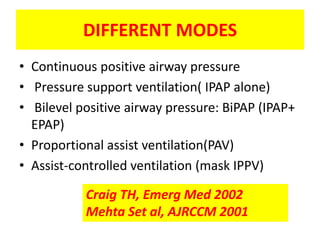
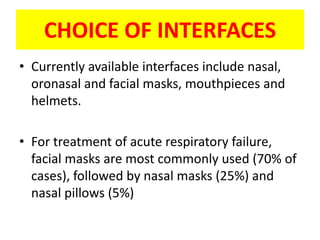
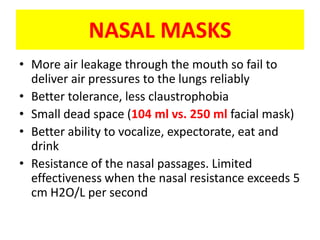
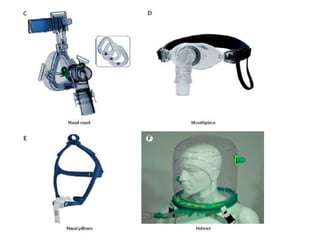
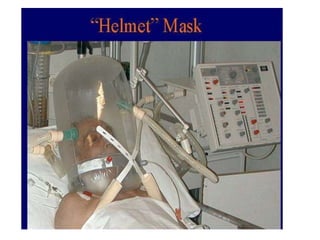
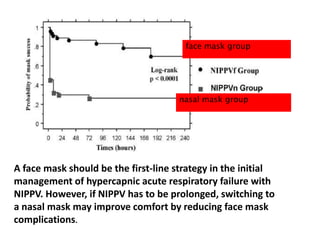
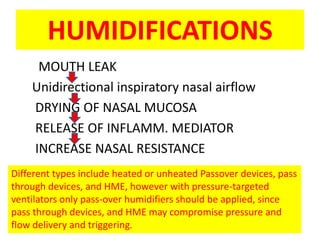
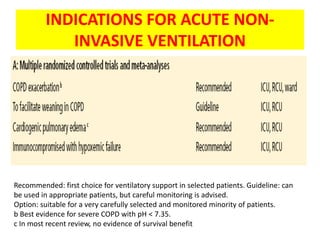
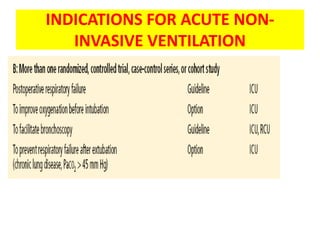
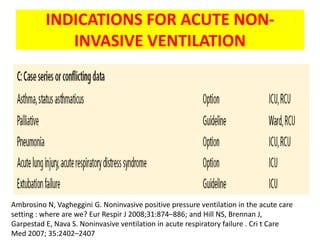
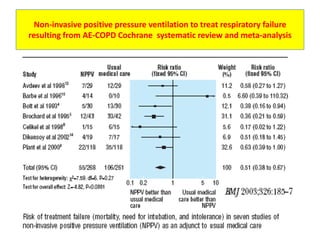
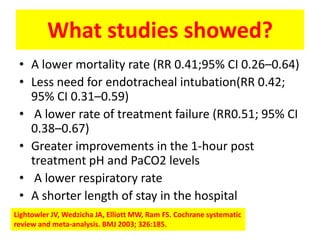
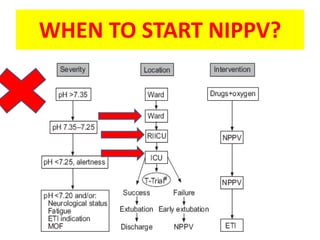
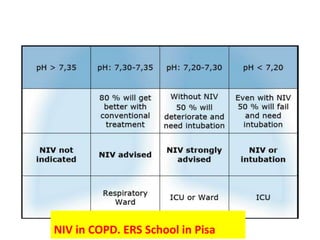
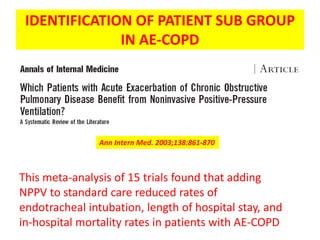
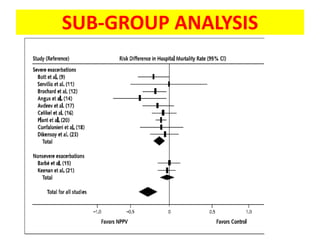
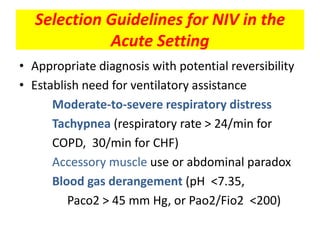
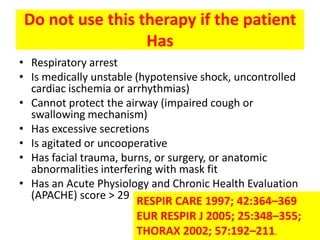
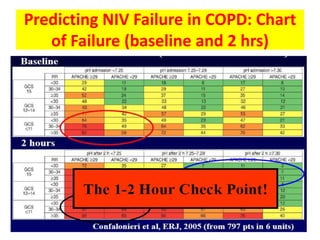
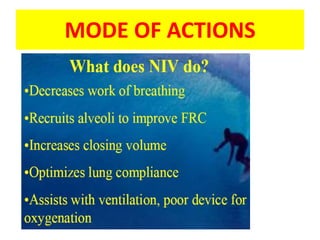
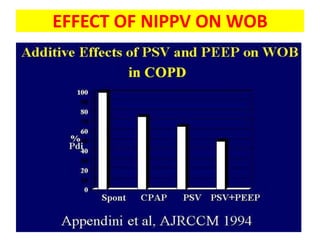
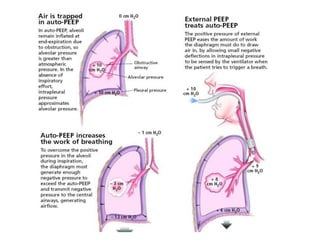
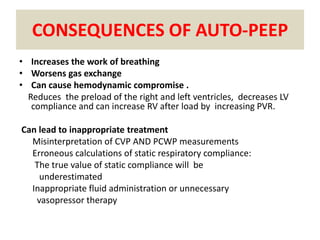
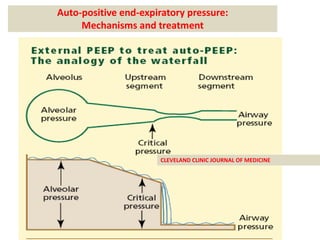
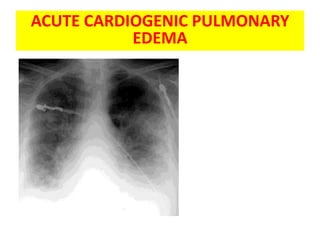
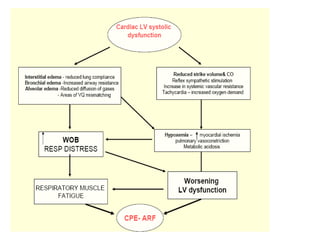
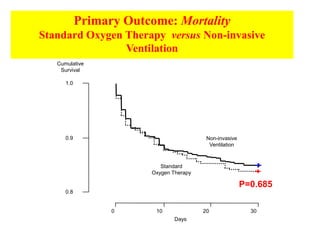
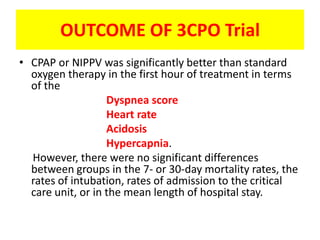
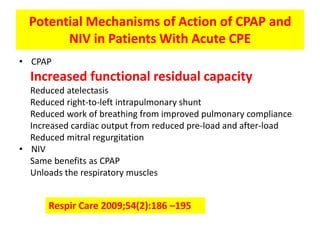
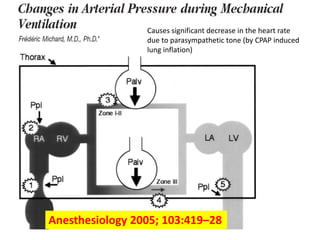
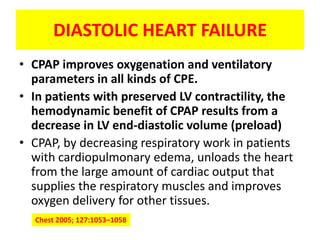
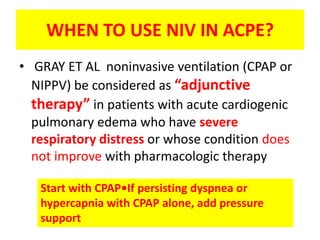
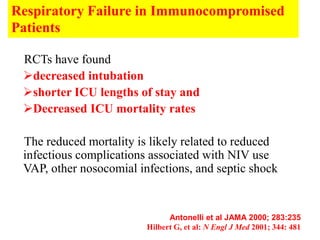
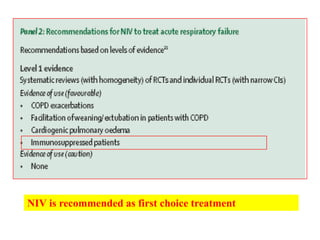
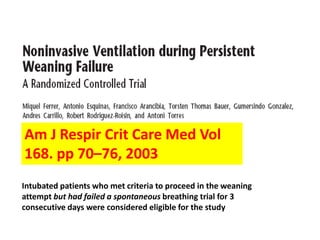
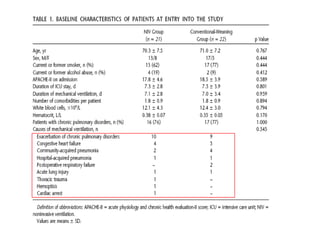
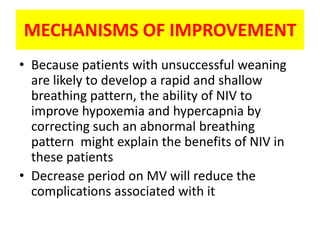
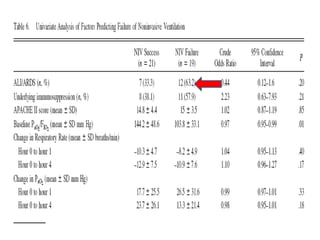
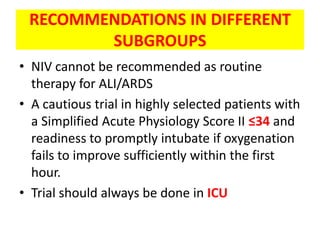
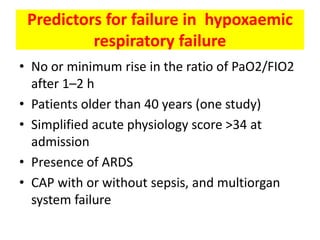
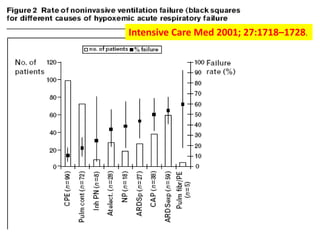
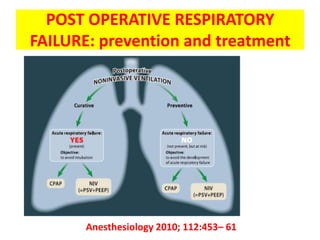
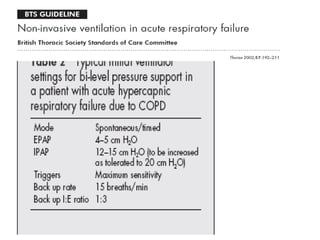
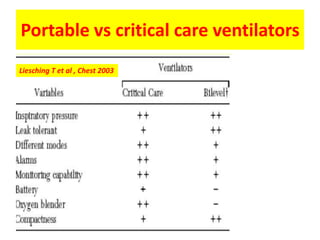
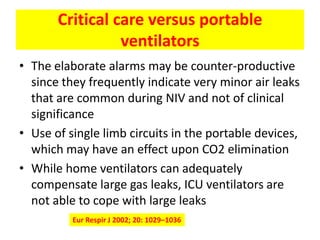
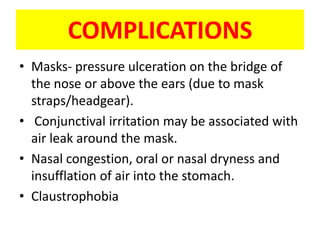
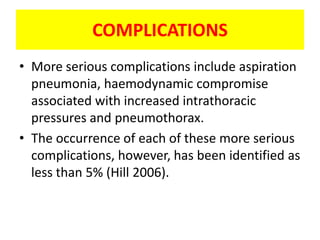
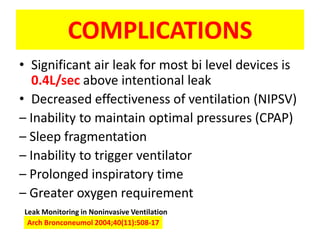
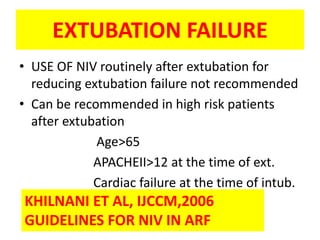
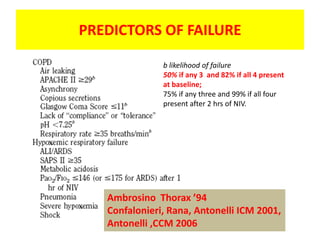
This document discusses non-invasive positive pressure ventilation (NIPPV). It defines NIPPV and describes its increasing importance and advantages over invasive ventilation. These advantages include avoiding intubation, reducing complications, decreasing ICU stay and costs. The document discusses the types of NIPPV, including negative pressure ventilation, continuous positive airway pressure, and noninvasive positive pressure ventilation. It covers interfaces, modes, humidification, and evidence-based guidelines for indications of NIPPV, including for acute exacerbations of COPD and acute cardiogenic pulmonary edema.