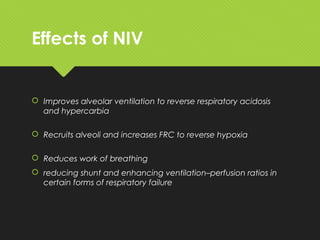
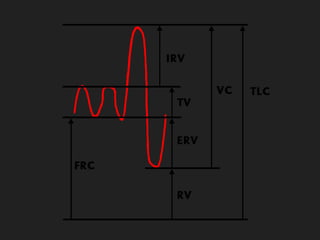
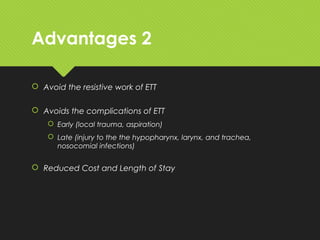
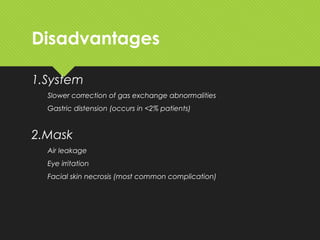
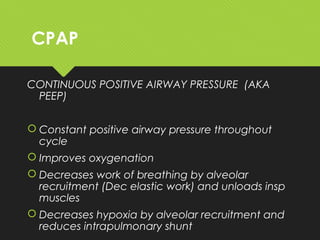
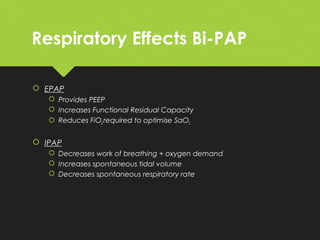
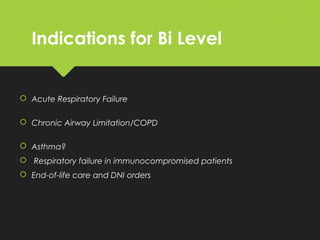
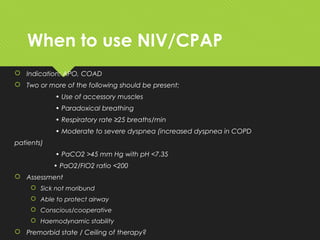
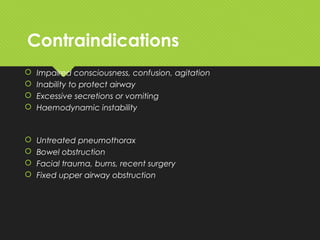
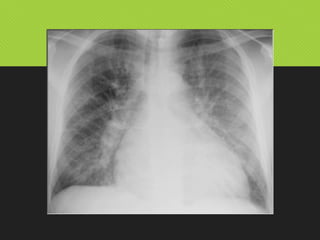
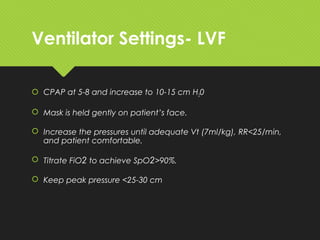
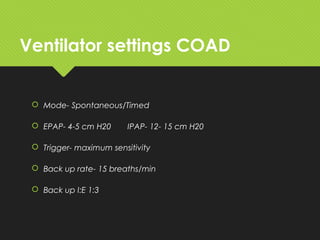
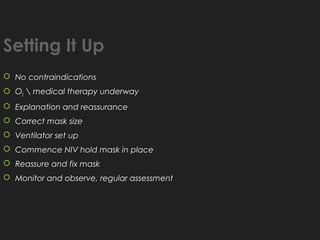
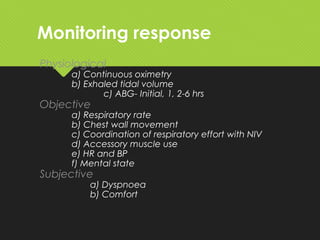
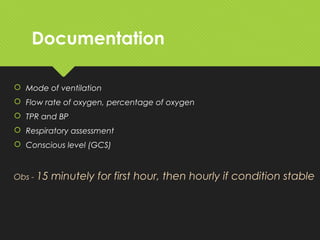
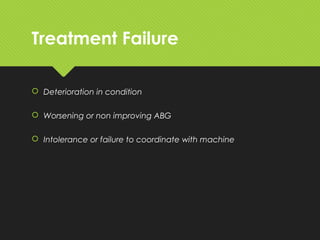
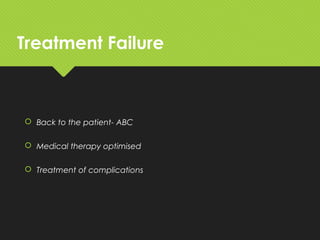
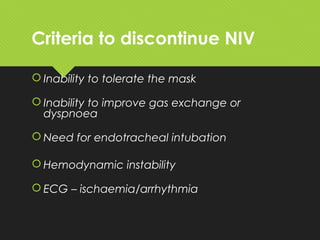
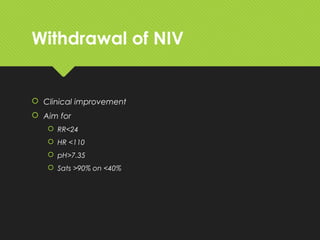
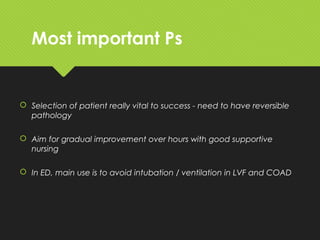
This document provides an overview of non-invasive ventilation. It discusses the history and development of respiratory support and mechanical ventilation. The objectives, definitions, theories, effects, advantages, disadvantages, indications, contraindications, modes, settings, monitoring, documentation, treatment failure criteria and discontinuation criteria of non-invasive ventilation are described. Key points include that non-invasive ventilation can avoid intubation for certain patients with acute respiratory failure from conditions like heart failure or COPD exacerbation. Close monitoring is required and intubation may still be necessary if the patient does not improve or their condition deteriorates.